Welcome to China Oncology,
China Oncology ›› 2023, Vol. 33 ›› Issue (2): 142-151.doi: 10.19401/j.cnki.1007-3639.2023.02.007
• Specialists' Article • Previous Articles Next Articles
CHEN Yuguang1,2( ), SUN Xiao2, BI Zhao1,2, QIU Pengfei1,2, DUAN Baowei1,2,3, FAN Qingda1,2, WANG Yongsheng1,2(
), SUN Xiao2, BI Zhao1,2, QIU Pengfei1,2, DUAN Baowei1,2,3, FAN Qingda1,2, WANG Yongsheng1,2( )
)
Received:2022-11-10
Revised:2023-02-07
Online:2023-02-28
Published:2023-03-22
Contact:
WANG Yongsheng
Share article
CLC Number:
CHEN Yuguang, SUN Xiao, BI Zhao, QIU Pengfei, DUAN Baowei, FAN Qingda, WANG Yongsheng. Internal mammary sentinel lymph node biopsy for breast cancer: a long-term follow-up research for assessment of prognosis and guiding individualized internal mammary lymph node irradiation[J]. China Oncology, 2023, 33(2): 142-151.
Tab.1
Demographic and clinical characteristics"
| Item | Case (n=537) | Percentage/% | Item | Case (n=537) | Percentage/% | |
|---|---|---|---|---|---|---|
| Age | 48.9±9.0 (27.0-78.0) | Grade | ||||
| BMI | 23.9±3.1 (16.4-39.7) | Ⅰ | 9 | 1.7 | ||
| Menopausal status | Ⅱ | 326 | 60.7 | |||
| No | 331 | 61.6 | Ⅲ | 163 | 30.3 | |
| Yes | 206 | 38.4 | N/A | 39 | 7.3 | |
| Laterality | No. of ALN positive | |||||
| Left | 305 | 56.8 | 0 | 263 | 49.0 | |
| Right | 232 | 43.2 | 1-3 | 173 | 32.2 | |
| Tumor location | 4-9 | 57 | 10.6 | |||
| Lateral | 282 | 52.5 | ≥10 | 44 | 8.2 | |
| Central/medial | 248 | 46.2 | IMSLN | |||
| Unknown | 7 | 1.3 | Negatvie | 440 | 81.9 | |
| Pathological size/cm | Positive | 97 | 18.1 | |||
| ≤2 | 271 | 50.4 | ER | |||
| 2-5 | 243 | 45.3 | Negatvie | 133 | 24.8 | |
| >5 | 23 | 4.3 | Positive | 404 | 75.2 | |
| Histological type | PR | |||||
| Ductal | 483 | 89.9 | Negatvie | 168 | 31.3 | |
| Lobular | 15 | 2.8 | Positive | 369 | 68.7 | |
| Mucinous | 8 | 1.5 | HER2 | |||
| Microinfiltration | 23 | 4.3 | Negatvie | 380 | 70.8 | |
| Other special types | 8 | 1.5 | Positive | 132 | 24.6 | |
| Lymphatic invasion | N/A | 25 | 4.6 | |||
| No | 465 | 86.6 | Tumor subtype | |||
| Yes | 72 | 13.4 | HR positive/HER2 negatvie | 316 | 58.8 | |
| No. of IMSLN | 1.8±0.9 (1-6) | HER2 positive | 132 | 24.6 | ||
| Surgery type | TNBC | 64 | 11.9 | |||
| Mastectomy | 502 | 93.5 | N/A | 25 | 4.7 | |
| Lumpectomy | 35 | 6.5 | ||||
Tab. 2
Univariate and multivariate Cox analysis for DFS and OS after IM-SLNB"
| Variables | DFS | OS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Cox analysis | Multivariate Cox analysis | Univariate Cox analysis | Multivariate Cox analysis | ||||||||
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | ||||
| IMSLN (positive vs negative) | 5.908 (3.194-10.928) | <0.001 | 3.652 (1.832-7.281) | <0.001 | 6.927 (2.783-17.240) | <0.001 | 3.232 (1.153-9.058) | 0.026 | |||
| Age | 0.994 (0.960-1.030) | 0.749 | 1.034 (0.984-1.086) | 0.190 | |||||||
| Menopausal status (yes vs no) | 1.338 (0.721-2.480) | 0.356 | 1.712 (0.694-4.222) | 0.243 | |||||||
| Tumor location (lateral vs central/medial) | 1.622 (0.871-3.020) | 0.127 | 1.993 (0.785-5.063) | 0.147 | |||||||
| No. of positive ALN | 1.121 (1.083-1.160) | <0.001 | 1.090 (1.045-1.137) | <0.001 | 1.138 (1.082-1.196) | <0.001 | 1.100 (1.032-1.173) | 0.003 | |||
| Pathological size (cm) | 0.002 | 0.006 | <0.001 | 0.013 | |||||||
| 2-5 (vs≤2) | 1.484 (0.760-2.899) | 0.248 | 0.769 (0.374-1.577) | 0.473 | 4.430 (1.250-15.700) | 0.021 | 2.597 (0.697-9.673) | 0.155 | |||
| >5 (vs≤2) | 5.367 (2.080-13.848) | <0.001 | 3.571 (1.357-9.395) | 0.010 | 17.214 (3.850-76.970) | <0.001 | 9.514 (2.023-44.749) | 0.004 | |||
| Histological grade (Ⅲ vs Ⅰ-Ⅱ) | 2.270 (1.230-4.189) | 0.009 | 2.367 (1.273-4.400) | 0.006 | 1.129 (0.429-2.973) | 0.806 | |||||
| Lymphatic invasion (yes vs no) | 1.106 (0.433-2.827) | 0.833 | 1.137 (0.261-4.945) | 0.864 | |||||||
| ER (ER+ vs ER-) | 0.550 (0.291-1.039) | 0.065 | 0.449 (0.180-1.115) | 0.085 | |||||||
| PR (PR+ vs PR-) | 0.668 (0.357-1.252) | 0.208 | 0.575 (0.231-1.429) | 0.233 | |||||||
| HER2 (HER2+ vs HER2-) | 1.171 (0.583-2.353) | 0.657 | 1.072 (0.386-2.979) | 0.893 | |||||||
| Tumor subtype | 0.219 | 0.209 | |||||||||
| HER2+ ( vs HR+/HER2-) | 1.372 (0.657-2.864) | 0.400 | 1.382 (0.463-4.124) | 0.562 | |||||||
| TN (vs HR+/HER2-) | 2.049 (0.902-4.653) | 0.087 | 2.683 (0.899-8.011) | 0.077 | |||||||
| Radiotherapy (yes vs no) | 1.384 0.731-2.621) | 0.319 | 1.856 (0.686-5.024) | 0.223 | |||||||
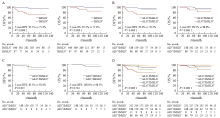
Fig. 1
Prognosis comparison of the different metastatic statuses of ALN/IMSLN Kaplan-Meier curves showed DFS and OS in all patients. 5-year DFS and OS were described. HR data were also shown. A: Kaplan-Meier DFS and OS in all patients with negative internal mammary sentinel lymph node (IMSLN negative; blue) and positive internal mammary sentinel lymph node (IMSLN positive, red); B: Kaplan-Meier DFS and OS in patients with IMSLN negative (blue) and IMSLN positive (red) in patients with positive axillary lymph nodes (ALN positive) (ALN positive/IMSLN negative vs ALN positive/IMSLN positive). C: Kaplan-Meier DFS and OS in patients with ALN negative/IMSLN negative (orange) and ALN positive/IMSLN positive (green); D: The DFS and OS of the 4 subgroups were shown on this graph. -: Negative; + : Positive."
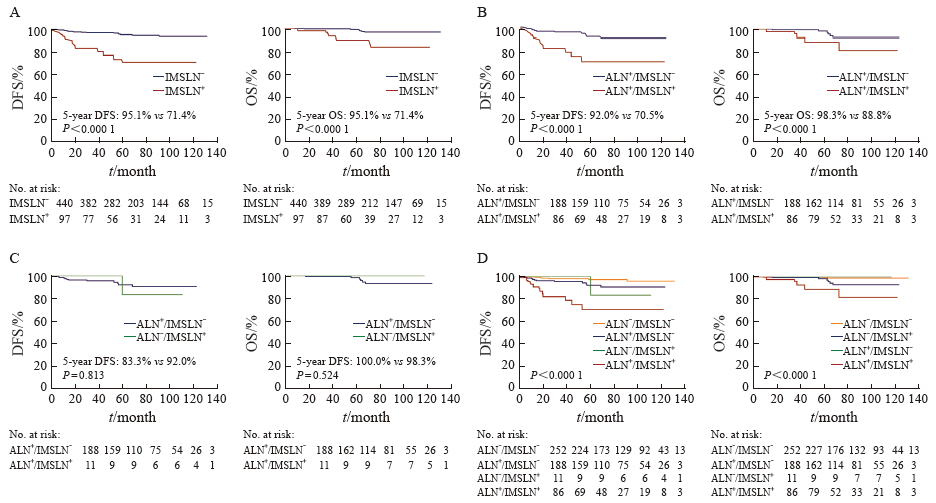
Fig. 2
Effects of IMNI on the prognosis of patients in different subgroups of IMSLN metastatic status Kaplan-Meier curves showed DFS and OS in all patients who have received radiation therapy. 5-year DFS were described. HR data were also shown. A: Kaplan-Meier DFS and OS in all patients with IMNI (red) and without IMNI (no IMNI, blue). B: Kaplan-Meier DFS and OS in IMSLN negative patients with IMNI (red) and without IMNI (no IMNI, blue). C: Kaplan-Meier DFS and OS in patients with IMSLN negative and ALN 1-3 positive with IMNI (red) and without IMNI (no IMNI, blue). D: Kaplan-Meier DFS and OS in patients with IMSLN-and ALN≥4 positive with IMNI (red) and without IMNI (no IMNI, blue). E: Kaplan-Meier DFS and OS in all IMSLN positive patients with IMNI (orange) and without IMNI (no IMNI, green). -: Negative; + : Positive."
Tab. 3
Hazard ratio (HR) for disease recurrence according to subgroups"
| Item | No IMNI (n=142) | IMNI (n=101) | 5-year DFS (IMNI vs no IMNI) | P value | HR (95% CI) |
|---|---|---|---|---|---|
| T1 | 47 | 39 | 91.9% vs 85.5% | 0.974 | 1.026 (0.228-4.617) |
| T2-3 | 95 | 62 | 84.7% vs 90.3% | 0.225 | 1.875 (0.680-5.175) |
| N1 | 109 | 41 | 100.0% vs 92.7% | 0.356 | 0.029 (0.000-52.000) |
| N2-3 | 29 | 60 | 77.4% vs 74.6% | 0.672 | 1.257 (0.435-3.633) |
| Ⅰ-Ⅱ | 100 | 26 | 100.0% vs 95.2% | 0.539 | 0.036 (0.000-1 486.000) |
| Ⅲ | 42 | 75 | 82.5% vs 74.6% | 0.919 | 0.952 (0.369-2.458) |
| Lateral | 84 | 43 | 87.9% vs 90.1% | 0.872 | 1.145 (0.218-6.009) |
| Central/medial | 54 | 57 | 83.4% vs 85.8% | 0.503 | 1.423 (0.506-3.998) |
| IMSLN positive | 19 | 67 | 87.3% vs 52.5% | 0.040 | 0.286 (0.087-0.943) |
| IMSLN negative | 123 | 34 | 84.5% vs 96.5% | 0.099 | 3.269 (0.488-21.890) |
Tab. 4
IMNI and radiation pneumonia"
| RILI | IMSLN- (n=157) | P value | OR (95% CI) | |||
|---|---|---|---|---|---|---|
| No IMNI (n=123) | IMNI (n=34) | |||||
| Grade 1-2 | Grade 3 | Grade 1-2 | Grade 3 | |||
| Acute pneumonitis | 7 (5.7%) | 0 (0.0%) | 3 (8.8%) | 0 (0.0%) | 0.883 | 1.465 (0.360-5.960) |
| Delayed pneumonitis or fibrosis | 10 (8.1%) | 0 (0.0%) | 10 (29.4%) | 0 (0.0%) | <0.050 | 4.708 (1.870-11.840) |
| Total | 17 (13.8%) | 13 (38.2%) | <0.050 | 3.678 (1.604-8.434) | ||
| RILI | IMSLN+ (n=86) | P value | OR (95% CI) | |||
| No IMNI (n=19) | IMNI (n=67) | |||||
| Grade 1-2 | Grade 3 | Grade 1-2 | Grade 3 | |||
| Acute pneumonitis | 0 (0.0%) | 0 (0.0%) | 8 (11.9%) | 0 (0.0%) | 0.252 | - |
| Delayed pneumonitis or fibrosis | 2 (10.5%) | 0 (0.0%) | 10 (14.9%) | 0 (0.0%) | 0.909 | 1.491 (0.300-7.410) |
| Total | 2 (10.5%) | 18(26.8%) | 0.234 | 3.122 (0.700-13.990) | ||
| [1] |
WHELAN T J, OLIVOTTO I A, PARULEKAR W R, et al. Regional nodal irradiation in early-stage breast cancer[J]. N Engl J Med, 2015, 373(4): 307-316.
doi: 10.1056/NEJMoa1415340 |
| [2] |
POORTMANS P M, WELTENS C, FORTPIED C, et al. Internal mammary and medial supraclavicular lymph node chain irradiation in stage Ⅰ-Ⅲ breast cancer (EORTC 22922/10925): 15-year results of a randomised, phase 3 trial[J]. Lancet Oncol, 2020, 21(12): 1602-1610.
doi: 10.1016/S1470-2045(20)30472-1 |
| [3] |
POORTMANS P M, COLLETTE S, KIRKOVE C, et al. Internal mammary and medial supraclavicular irradiation in breast cancer[J]. N Engl J Med, 2015, 373(4): 317-327.
doi: 10.1056/NEJMoa1415369 |
| [4] |
THORSEN L B J, OVERGAARD J, MATTHIESSEN L W, et al. Internal mammary node irradiation in patients with node-positive early breast cancer: fifteen-year results from the Danish breast cancer group internal mammary node study[J]. J Clin Oncol, 2022, 40(36): 4198-4206.
doi: 10.1200/JCO.22.00044 |
| [5] |
HENNEQUIN C, BOSSARD N, SERVAGI-VERNAT S, et al. Ten-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomy[J]. Int J Radiat Oncol Biol Phys, 2013, 86(5): 860-866.
doi: 10.1016/j.ijrobp.2013.03.021 |
| [6] |
BUDACH W, KAMMERS K, BOELKE E, et al. Adjuvant radiotherapy of regional lymph nodes in breast cancer - a meta-analysis of randomized trials[J]. Radiat Oncol, 2013, 8: 267.
doi: 10.1186/1748-717X-8-267 pmid: 24225206 |
| [7] |
CONG B B, CAO X S, CAO L, et al. Internal mammary lymph nodes radiotherapy of breast cancer in the era of individualized medicine[J]. Oncotarget, 2017, 8(46): 81583-81590.
doi: 10.18632/oncotarget.v8i46 |
| [8] |
QIU P F, WANG X E, WANG Y S. Indications for individual internal mammary node irradiation[J]. Lancet Oncol, 2021, 22(2): e40.
doi: 10.1016/S1470-2045(20)30739-7 |
| [9] |
邱鹏飞, 王永胜. 前哨淋巴结时代乳腺癌的精准区域处理: 演进与展望[J]. 中国癌症杂志, 2022, 32(8): 680-687.
doi: 10.19401/j.cnki.1007-3639.2022.08.002 |
| QIU P F, WANG Y S. Precise regional management of breast cancer in the sentinel lymph node era: evolution and prospect[J]. China Oncol, 2022, 32(8): 680-687. | |
| [10] |
QIU P F, LIU J J, LIU Y B, et al. A modified technology could significantly improve the visualization rate of the internal mammary sentinel lymph nodes in breast cancer patients[J]. Breast Cancer Res Treat, 2012, 136(1): 319-321.
doi: 10.1007/s10549-012-2203-5 |
| [11] |
QIU P F, WANG Y S. ASO author reflections: internal mammary sentinel lymph node biopsy-time for the back of internal mammary staging?[J]. Ann Surg Oncol, 2020, 27(2): 384-385.
doi: 10.1245/s10434-019-07838-2 |
| [12] |
VERONESI U, CASCINELLI N, BUFALINO R, et al. Risk of internal mammary lymph node metastases and its relevance on prognosis of breast cancer patients[J]. Ann Surg, 1983, 198(6): 681-684.
doi: 10.1097/00000658-198312000-00002 pmid: 6639172 |
| [13] |
KIM Y B, BYUN H K, KIM D Y, et al. Effect of elective internal mammary node irradiation on disease-free survival in women with node-positive breast cancer: a randomized phase 3 clinical trial[J]. JAMA Oncol, 2022, 8(1): 96-105.
doi: 10.1001/jamaoncol.2021.6036 |
| [14] |
MATZINGER O, HEIMSOTH I, POORTMANS P, et al. Toxicity at three years with and without irradiation of the internal mammary and medial supraclavicular lymph node chain in stage Ⅰ to Ⅲ breast cancer (EORTC trial 22922/10925)[J]. Acta Oncol, 2010, 49(1): 24-34.
doi: 10.3109/02841860903352959 |
| [15] |
POORTMANS P M, STRUIKMANS H, DE BROUWER P, et al. Side effects 15 years after lymph node irradiation in breast cancer: randomized EORTC trial 22922/10925[J]. J Natl Cancer Inst, 2021, 113(10): 1360-1368.
doi: 10.1093/jnci/djab113 |
| [16] |
THORSEN L B, THOMSEN M S, BERG M, et al. CT-planned internal mammary node radiotherapy in the DBCG-IMN study: benefit versus potentially harmful effects[J]. Acta Oncol, 2014, 53(8): 1027-1034.
doi: 10.3109/0284186X.2014.925579 pmid: 24957557 |
| [17] |
CAO X S, YANG G R, CONG B B, et al. The lymphatic drainage pattern of internal mammary sentinel lymph node identified by small particle radiotracer (99mTc-dextran 40) in breast[J]. Cancer Res Treat, 2019, 51(2): 483-492.
doi: 10.4143/crt.2018.062 |
| [18] |
CONG B B, QIU P F, LIU Y B, et al. Validation study for the hypothesis of internal mammary sentinel lymph node lymphatic drainage in breast cancer[J]. Oncotarget, 2016, 7(27): 41996-42006.
doi: 10.18632/oncotarget.v7i27 |
| [19] | 邱鹏飞. 新型示踪技术引导乳腺癌内乳前哨淋巴结活检术的显像率与适应证研究[D]. 济南: 山东大学, 2020. |
| [20] | 孙晓. 乳腺癌内乳区前哨淋巴结活检术的前瞻性临床验证研究[D]. 济南: 山东大学, 2020. |
| [21] | WANG Y S, LV Q, ZHU S G, et al. Prospective, multicenter, clinical validation study of the repeatability and accuracy of internal mammary sentinel lymph node biopsy with modified injection technique (CBCSG026/CBCSG027)[C]. 2022 San Antonio Breast Cancer Symposium; San Antonio, TX, Dec 6-10, 2022 (abstr P2-14-06). |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
