Welcome to China Oncology,
China Oncology ›› 2024, Vol. 34 ›› Issue (7): 650-658.doi: 10.19401/j.cnki.1007-3639.2024.07.004
• Article • Previous Articles Next Articles
JIANG Dan1( ), SONG Guoqing1(
), SONG Guoqing1( ), WANG Xiaodan2
), WANG Xiaodan2
Received:2023-10-30
Revised:2024-06-15
Online:2024-07-30
Published:2024-08-08
Contact:
SONG Guoqing
Share article
CLC Number:
JIANG Dan, SONG Guoqing, WANG Xiaodan. Study on the mechanism of mitochondrial dysfunction and CPT1A/ERK signal transduction pathway regulating malignant behavior in breast cancer[J]. China Oncology, 2024, 34(7): 650-658.

Fig. 1
Abnormal expression of CPT1A in breast cancer tissue promotes tumor metastasis A, B: The expression of CPT1A mRNA in breast cancer tissues (n=1 085), normal breast tissues (n=291) and breast cancer tissues with different stages was analyzed by GEPIA. C: Using TCGA GEPIA to generate Kaplan-Meier diagram of breast cancer patients. The data of 1 069 breast cancer patients were divided into two groups according to the median percentile of CPT1A expression. D, E: Western blot representation and quantitative analysis of the expression level of CPT1A after overexpression. F, G: Transwell were used to determine the invasive ability of breast cancer cells expressing CPT1A or negative control vector. H, I: Western blot representation and quantitative analysis of the expression level of CPT1A after shRNA knockdown. J, K: Transwell were used to determine the invasive ability of breast cancer cells or negative control cells after CPT1A knock-down. *: P<0.05, compared with normal breast tissues; ***: P<0.001, compared with NC group."
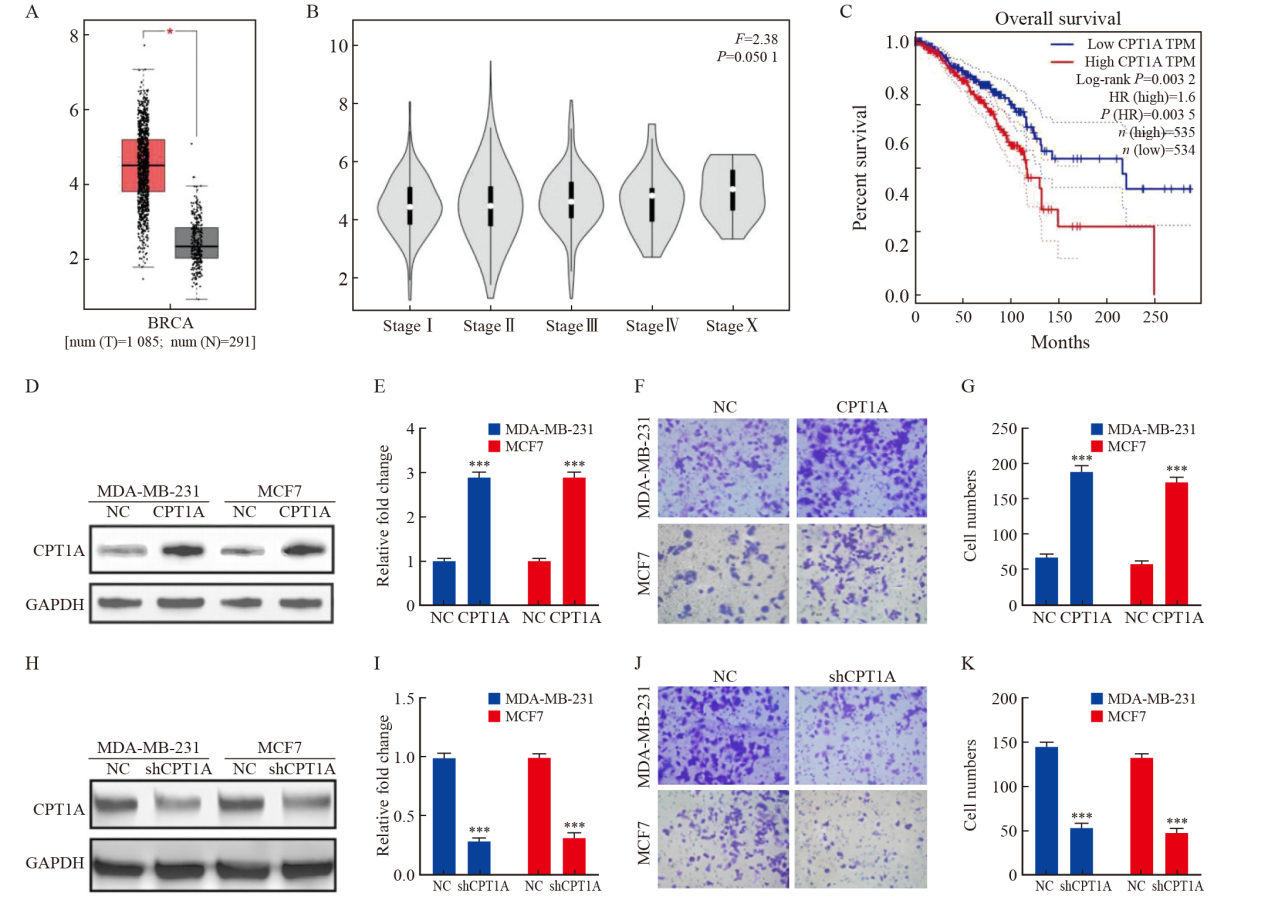
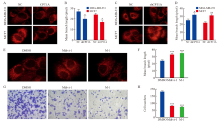
Fig. 2
CPT1A promotes breast cancer cell metastasis by regulating mitochondrial division A, B: Mitotracker living cell mitochondrial imaging and average mitochondrial branch length of cells overexpressing CPT1A or negative control. C, D: Mitotracker living cell mitochondrial imaging and average mitochondrial branch length of shRNA knock-down or negative control cells. E, F: Mitotracker mitochondrial imaging and average mitochondrial branching length of CPT1A overexpressing MDA-MB-231 cells treated with Mdivi-1 and M-1. G, H: Transwell was used to determine the invasive ability of CPT1A cells overexpressed MDA-MB-231 treated with Mdivi-1 and M-1. *: P<0.05, compared with NC group; **: P<0.01, compared with NC group; ***: P<0.001, compared with DMSO group."
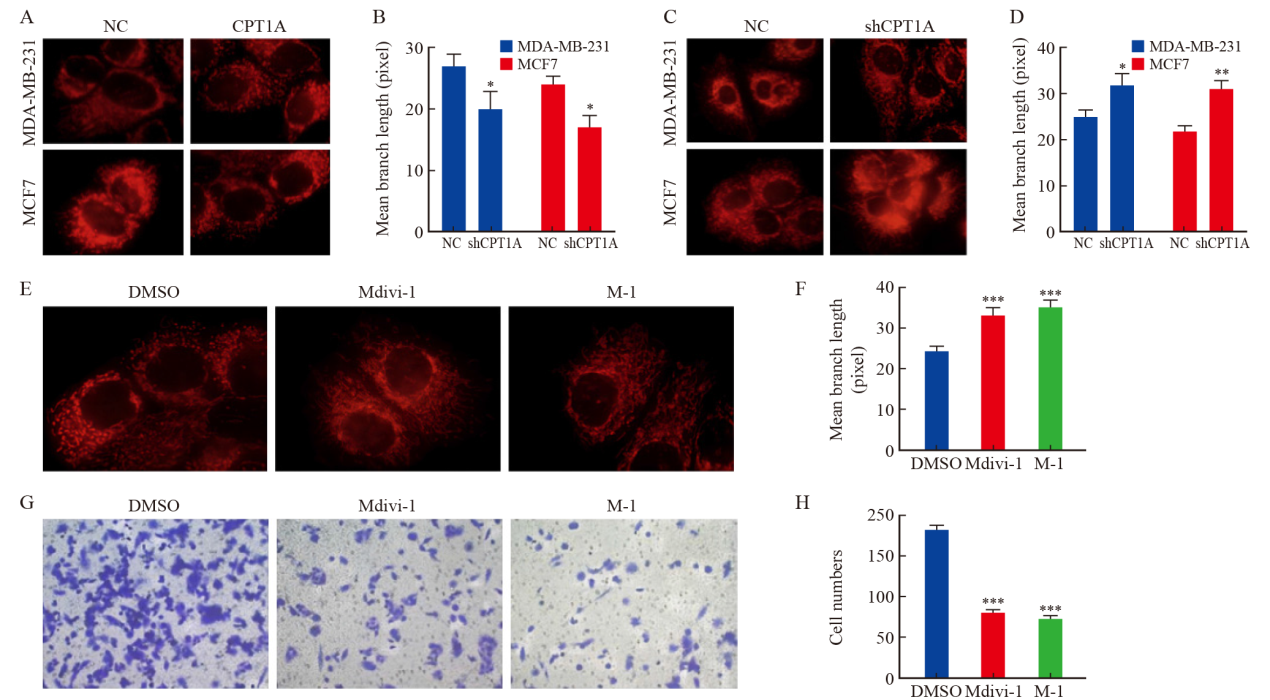
Fig. 3
CPT1A activates PGC-1α through ERK1/2 A: Antibody array scanning of MDA-MB-231 cells overexpressing CPT1A. B, C: Western blot analysis and quantitative analysis of ERK1/2-PGC-1α expression in MDA-MB-231 cells over-expressing CPT1A. D, E: Western blot analysis and quantitative analysis of ERK1/2-PGC-1α expression in MDA-MB-231 cells treated with different doses of PD325901 for 8 h. *: P<0.05, compared with 0 nmol/L group; **: P<0.01, compared with NC group or 0 nmol/L group; ***: P<0.001, compared with NC group or 0 nmol/L group."
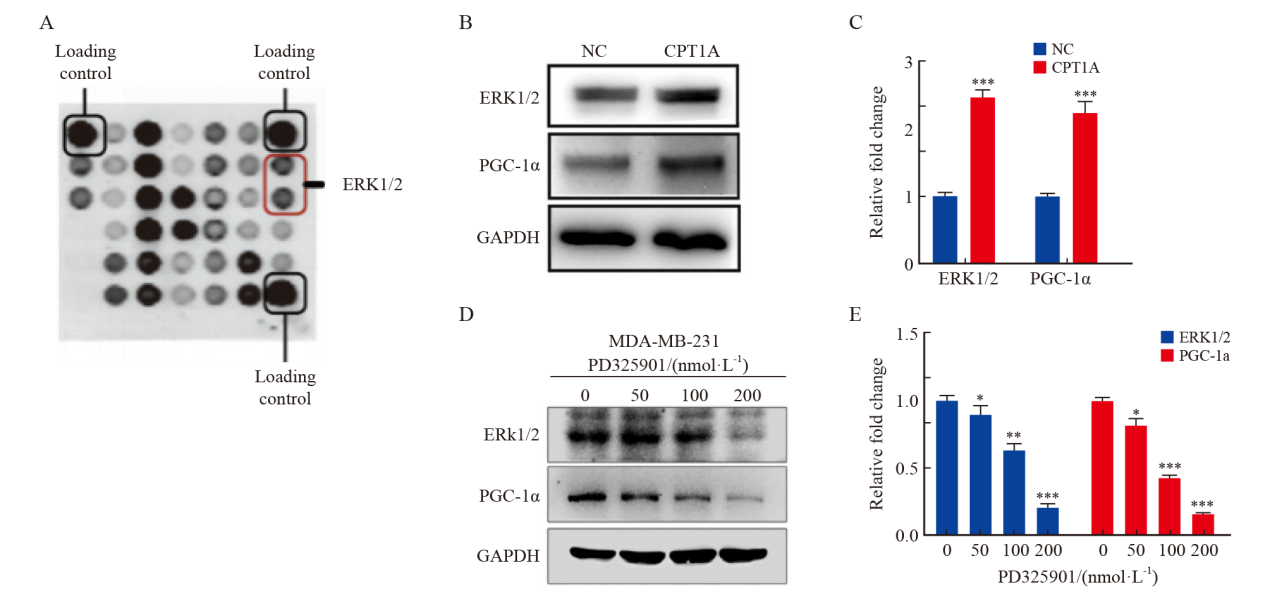
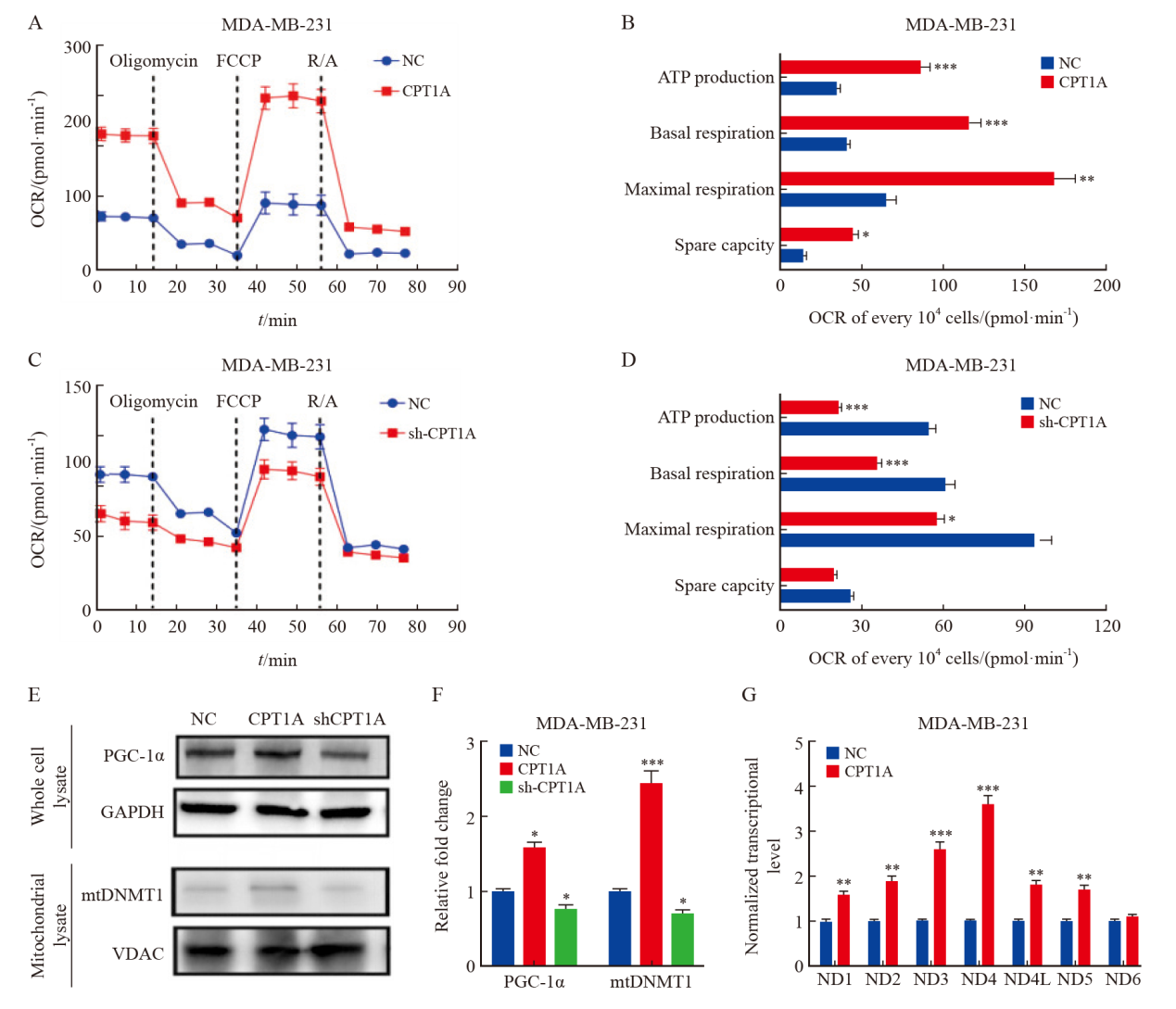
Fig. 4
CPT1A promotes mitochondrial oxidative phosphorylation A, B: Real-time OCR tracing of MDA-MB-231 cells overexpressing CPT1A and negative control and statistics of respiratory parameters. C, D: Real-time OCR tracing of MDA-MB-231 cells with CPT1A knockdown and negative control and statistics of respiratory parameters. E, F: Western blot analysis of the expression and quantitative analysis of PGC-1α and mitochondrial DNMT1 in MDA-MB-231 cells that overexpressed CPT1A and knocked down CPT1A. G: The expression level of mitochondrial DNA coding gene was measured by Taqman assay, and the data was standardized to 18s rRNA. *: P<0.05, compared with NC group; **: P<0.01, compared with NC group; ***: P<0.001, compared with NC group."
| [1] | GIAQUINTO A N, SUNG H, MILLER K D, et al. Breast cancer statistics, 2022[J]. CA Cancer J Clin, 2022, 72(6): 524-541. |
| [2] | XIA C F, DONG X S, LI H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants[J]. Chin Med J, 2022, 135(5): 584-590. |
| [3] | GALIANDRO F, AGNES S, MOSCHETTA G, et al. Prognostic factors in patients with breast cancer liver metastases undergoing liver resection: systematic review and meta-analysis[J]. Cancers, 2022, 14(7): 1691. |
| [4] | KOTECHA R, TONSE R, RUBENS M, et al. Systematic review and meta-analysis of breast cancer brain metastasis and primary tumor receptor expression discordance[J]. Neurooncol Adv, 2021, 3(1): vdab010. |
| [5] | VONA R, MILEO A M, MATARRESE P. Microtubule-based mitochondrial dynamics as a valuable therapeutic target in cancer[J]. Cancers, 2021, 13(22): 5812. |
| [6] | KUMAR H, GUPTA N V, JAIN R, et al. A review of biological targets and therapeutic approaches in the management of triple-negative breast cancer[J]. J Adv Res, 2023, 54: 271-292. |
| [7] | JIANG N, XING B Z, PENG R, et al. Inhibition of Cpt1a alleviates oxidative stress-induced chondrocyte senescence via regulating mitochondrial dysfunction and activating mitophagy[J]. Mech Ageing Dev, 2022, 205: 111688. |
| [8] |
SAVUKAITYTĖ A, BARTNYKAITĖ A, BEKAMPYTĖ J, et al. DDIT4 downregulation by siRNA approach increases the activity of proteins regulating fatty acid metabolism upon aspirin treatment in human breast cancer cells[J]. Curr Issues Mol Biol, 2023, 45(6): 4665-4674.
doi: 10.3390/cimb45060296 pmid: 37367045 |
| [9] | JOSHI M, KIM J, D’ALESSANDRO A, et al. CPT1A over-expression increases reactive oxygen species in the mitochondria and promotes antioxidant defenses in prostate cancer[J]. Cancers, 2020, 12(11): 3431. |
| [10] |
DAS M, GIANNOUDIS A, SHARMA V. The role of CPT1A as a biomarker of breast cancer progression: a bioinformatic approach[J]. Sci Rep, 2022, 12(1): 16441.
doi: 10.1038/s41598-022-20585-x pmid: 36180554 |
| [11] | ZHANG W, DU X F, LIU B, et al. Engineering supramolecular nanomedicine for targeted near infrared-triggered mitochondrial dysfunction to potentiate cisplatin for efficient chemophototherapy[J]. ACS Nano, 2022, 16(1): 1421-1435. |
| [12] | FORTE M, SCHIRONE L, AMERI P, et al. The role of mitochondrial dynamics in cardiovascular diseases[J]. Br J Pharmacol, 2021, 178(10): 2060-2076. |
| [13] | YOU Y, MURAOKA S, JEDRYCHOWSKI M P, et al. Human neural cell type-specificextracellular vesicle proteome defines disease-related molecules associated with activated astrocytes in Alzheimer’s disease brain[J]. J Extracell Vesicles, 2022, 11(1): e12183. |
| [14] | ANSARI M I, BANO N, KAINAT K M, et al. Bisphenol A exposure induces metastatic aggression in low metastatic MCF-7 cells via PGC-1α mediated mitochondrial biogenesis and epithelial-mesenchymal plasticity[J]. Life Sci, 2022, 302: 120649. |
| [15] | MIDDLETON P, VERGIS N. Mitochondrial dysfunction and liver disease: role, relevance, and potential for therapeutic modulation[J]. Therap Adv Gastroenterol, 2021, 14: 17562848211031394. |
| [16] |
LIU Y E, SHI Y F. Mitochondria as a target in cancer treatment[J]. MedComm, 2020, 1(2): 129-139.
doi: 10.1002/mco2.16 pmid: 34766113 |
| [17] | LEE K M, GILTNANE J M, BALKO J M, et al. MYC and MCL1 cooperatively promote chemotherapy-resistant breast cancer stem cells via regulation of mitochondrial oxidative phosphorylation[J]. Cell Metab, 2017, 26(4): 633-647. e7. |
| [18] | PRAHARAJ P P, PATRO B S, BHUTIA S K. Dysregulation of mitophagy and mitochondrial homeostasis in cancer stem cells: novel mechanism for anti-cancer stem cell-targeted cancer therapy[J]. Br J Pharmacol, 2022, 179(22): 5015-5035. |
| [19] | ZHANG L, SUN L, WANG L R, et al. Mitochondrial division inhibitor (mdivi-1) inhibits proliferation and epithelial-mesenchymal transition via the NF-κB pathway in thyroid cancer cells[J]. Toxicol In Vitro, 2023, 88: 105552. |
| [20] |
RANA A, OLIVEIRA M P, KHAMOUI A V, et al. Promoting Drp1-mediated mitochondrial fission in midlife prolongs healthy lifespan of drosophila melanogaster[J]. Nat Commun, 2017, 8(1): 448.
doi: 10.1038/s41467-017-00525-4 pmid: 28878259 |
| [21] | HU N, CHEN X M, CHEN C C, et al. Exploring the role of esketamine in alleviating depressive symptoms in mice via the PGC-1α/irisin/ERK1/2 signaling pathway[J]. Sci Rep, 2023, 13(1): 16611. |
| [22] |
HUANG K Y, LIU Z Y, XIE Z L, et al. HIGD2A silencing impairs hepatocellular carcinoma growth via inhibiting mitochondrial function and the MAPK/ERK pathway[J]. J Transl Med, 2023, 21(1): 253.
doi: 10.1186/s12967-023-04105-7 pmid: 37041638 |
| [23] |
LIU J F, NING L. Protective role of emodin in rats with post-myocardial infarction heart failure and influence on extracellular signal-regulated kinase pathway[J]. Bioengineered, 2021, 12(2): 10246-10253.
doi: 10.1080/21655979.2021.1983977 pmid: 34839778 |
| [24] | LAURIN K M, COUTU-BEAUDRY K, SALAZAR A, et al. Low expression of PGC-1β and other mitochondrial biogenesis modulators in melanoma is associated with growth arrest and the induction of an immunosuppressive gene expression program dependent on MEK and IRF-1[J]. Cancer Lett, 2022, 541: 215738. |
| [25] | ASL E R, AMINI M, NAJAFI S, et al. Interplay between MAPK/ERK signaling pathway and microRNAs: a crucial mechanism regulating cancer cell metabolism and tumor progression[J]. Life Sci, 2021, 278: 119499. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
