Welcome to China Oncology,
China Oncology ›› 2025, Vol. 35 ›› Issue (2): 228-236.doi: 10.19401/j.cnki.1007-3639.2025.02.010
• Specialist's Article • Previous Articles Next Articles
LU Yongjin1,2( ), SHI Zhiqiang1, LI Tong3, WANG Yongsheng1, QIU Pengfei1,2(
), SHI Zhiqiang1, LI Tong3, WANG Yongsheng1, QIU Pengfei1,2( )
)
Received:2024-12-27
Revised:2025-01-21
Online:2025-02-28
Published:2025-03-19
Supported by:Share article
CLC Number:
LU Yongjin, SHI Zhiqiang, LI Tong, WANG Yongsheng, QIU Pengfei. Retrospective study on regional lymph node radiotherapy after axillary dissection exemption in breast cancer patients with sentinel lymph node positive status[J]. China Oncology, 2025, 35(2): 228-236.
Tab. 1
Basic characteristics of the patient"
| RNI (n=186) | No-RNI (n=170) | P value | RNI (n=186) | No-RNI (n=170) | P value | |||
|---|---|---|---|---|---|---|---|---|
| Age/year | 0.093 | Vascular invasion | 0.098 | |||||
| Median | 47 (30-75) | 49 (27-75) | Yes | 59 (31.7%) | 40 (23.5%) | |||
| BMI | 0.173 | No | 127 (68.3%) | 130 (76.5%) | ||||
| Median | 24.24 (16.73-39.79) | 24.59 (17.22-38.87) | Estrogen receptor | 0.438 | ||||
| Menopause status | 0.828 | Negative | 28 (15.1%) | 20 (11.8%) | ||||
| Premenopausal | 116 (62.4%) | 104 (61.2%) | Positive | 158 (84.9%) | 150 (88.2%) | |||
| Postmenopausal | 70 (37.6%) | 66 (38.8%) | Progesterone receptor | 0.428 | ||||
| Laterality | 0.168 | Negative | 41 (22.0%) | 31 (18.2%) | ||||
| Left | 103 (55.4%) | 81 (47.6%) | Positive | 145 (78.0%) | 139 (81.8%) | |||
| Right | 83 (44.6%) | 89 (52.4%) | HER-2 | 0.143 | ||||
| Tumor location | 0.116 | Negative | 152 (81.7%) | 149 (87.6%) | ||||
| Lateral | 116 (62.4%) | 120 (70.6%) | Positive | 34 (18.3%) | 21 (12.4%) | |||
| Central/medial | 70 (37.6%) | 50 (29.4%) | Positive number of SLN | 0.006 | ||||
| Tumour size D/cm | 0.043 | 1 | 136 (73.1%) | 147 (86.5%) | ||||
| ≤2.0 | 101 (54.3%) | 112 (65.9%) | 2 | 42 (22.6%) | 20 (11.8%) | |||
| 2.0<D≤5.0 | 80 (43.0%) | 57 (33.5%) | 3 | 8 (4.3%) | 3 (1.8%) | |||
| >5.0 | 5 (2.7%) | 1(0.6%) | Type of surgery | <0.001 | ||||
| Histological type | 0.299 | TM | 133 (71.5%) | 35 (20.6%) | ||||
| IDC | 176 (94.6%) | 156 (91.8%) | BCS | 53 (28.5%) | 135 (79.4%) | |||
| Others | 10 (5.4%) | 14 (8.2%) | ||||||
| Histologic grade | 0.139 | |||||||
| Ⅰ | 2 (1.1%) | 2 (1.2%) | ||||||
| Ⅱ | 127 (68.3%) | 104 (61.2%) | ||||||
| Ⅲ | 51 (27.4%) | 49 (28.8%) | ||||||
| NA | 6 (3.2%) | 15 (8.8%) |
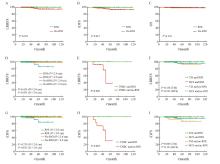
Fig. 2
Kaplan-Meier curves for survival analysis of breast cancer patients based on receipt of RNI The Kaplan-Meier curves illustrated LRRFS, iDFS, and OS for the patients. The first row presented the Kaplan-Meier curves for LRRFS (A), iDFS (B), and OS (C) comparing the RNI group (green) and the no-RNI group (red) in all patients. The second and third rows showed exploratory subgroup analyses of LRRFS and iDFS for different patient subgroups. D-G: Tumor size subgroups (R≤2 cm/RNI: Green; R>2 cm/RNI: Red; R≤ 2 cm/no-RNI: Orange; R>2 cm/no-RNI: Blue). E-H: Kaplan-Meier LRRFS and iDFS for triple-negative breast cancer (TNBC) patients (RNI: Green; no-RNI: Red). F, I: Surgical approach subgroups (TM/RNI: Green; BCS/RNI: Red; TM/no-RNI: Orange; BCS/no-RNI: Blue)."

| [1] | 李培, 吴炅. 中国乳腺癌外科治疗现状和新趋势[J]. 中国肿瘤临床, 2022, 49(22): 1151-1155. |
| LI P, WU J. Current status and new trends of surgical treatment for breast cancer in China[J]. Chin J Clin Oncol, 2022, 49(22): 1151-1155. | |
| [2] |
GIULIANO A E, KIRGAN D M, GUENTHER J M, et al. Lymphatic mapping and sentinel lymphadenectomy for breast cancer[J]. Ann Surg, 1994, 220(3): 391-398;discussion, 398-401.
doi: 10.1097/00000658-199409000-00015 pmid: 8092905 |
| [3] |
POODT I G M, SPRONK P E R, VUGTS G, et al. Trends on axillary surgery in nondistant metastatic breast cancer patients treated between 2011 and 2015: a Dutch population-based study in the ACOSOG-Z0011 and AMAROS era[J]. Ann Surg, 2018, 268(6): 1084-1090.
doi: 10.1097/SLA.0000000000002440 pmid: 28742702 |
| [4] | GARCIA-ETIENNE C A, MANSEL R E, TOMATIS M, et al. Trends in axillary lymph node dissection for early-stage breast cancer in Europe: impact of evidence on practice[J]. Breast, 2019, 45: 89-96. |
| [5] |
DONKER M, VAN TIENHOVEN G, STRAVER M E, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial[J]. Lancet Oncol, 2014, 15(12): 1303-1310.
doi: 10.1016/S1470-2045(14)70460-7 pmid: 25439688 |
| [6] | GIULIANO A E, BALLMAN K V, MCCALL L, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (alliance) randomized clinical trial[J]. JAMA, 2017, 318(10): 918-926. |
| [7] |
GALIMBERTI V, COLE B F, VIALE G, et al. Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23-01): 10-year follow-up of a randomised, controlled phase 3 trial[J]. Lancet Oncol, 2018, 19(10): 1385-1393.
doi: S1470-2045(18)30380-2 pmid: 30196031 |
| [8] | GIULIANO A E, HUNT K K, BALLMAN K V, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial[J]. JAMA, 2011, 305(6): 569-575. |
| [9] |
JAGSI R, CHADHA M, MONI J, et al. Radiation field design in the ACOSOG Z0011 (alliance) trial[J]. J Clin Oncol, 2014, 32(32): 3600-3606.
doi: 10.1200/JCO.2014.56.5838 pmid: 25135994 |
| [10] | BARTELS S A L, DONKER M, PONCET C, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer: 10-year results of the randomized controlled EORTC 10981-22023 AMAROS trial[J]. J Clin Oncol, 2023, 41(12): 2159-2165. |
| [11] | DE BONIFACE J, TVEDSKOV T F, RYDÉN L, et al. Omitting axillary dissection in breast cancer with sentinel-node metastases[J]. N Engl J Med, 2024, 390(13): 1163-1175. |
| [12] | 袁芊芊, 侯晋轩, 苏科华, 等. 基于上肢淋巴引流的乳腺癌术后水肿风险因素分析[J]. 中华普通外科杂志, 2021, 36(8): 579-584. |
| YUAN Q Q, HOU J X, SU K H, et al. Risk factors analysis of breast cancer-related lymphedema based on the proportion of the arm lymph flow above and below the axillary vein[J]. Chin J Gen Surg, 2021, 36(8): 579-584. | |
| [13] | 毕钊, 王永胜, 邱鹏飞. 2024版NCCN乳腺癌临床实践指南更新解读[J]. 中国肿瘤外科杂志, 2024, 16(5): 417-422. |
| BI Z, WANG Y S, QIU P F. Update and interpretation of NCCN clinical practice guidelines for breast cancer in 2024 edition[J]. Chin J Surg Oncol, 2024, 16(5): 417-422. | |
| [14] | 杨成林, 李建彬, 王玮. 乳腺癌术后放疗与全身系统治疗的顺序选择[J]. 中华放射医学与防护杂志, 2021, 41(10): 790-795. |
| YANG C L, LI J B, WANG W. Sequence selection of postoperative radiotherapy and systemic treatment for breast cancer patients[J]. Chin J Radiol Med Prot, 2021, 41(10): 790-795. | |
| [15] |
毕钊, 王永胜. 1-2枚前哨淋巴结阳性早期乳腺癌患者治疗策略降阶梯新理念[J]. 中国癌症杂志, 2023, 33(6): 560-565.
doi: 10.19401/j.cnki.1007-3639.2023.06.002 |
| BI Z, WANG Y S. New concept of de-escalation management strategy in breast cancer patients with 1-2 positive sentinel lymph nodes[J]. China Oncol, 2023, 33(6): 560-565. | |
| [16] | SÁVOLT Á, PÉLEY G, POLGÁR C, et al. Eight-year follow up result of the OTOASOR trial: the optimal treatment of the axilla-surgery or radiotherapy after positive sentinel lymph node biopsy in early-stage breast cancer a randomized, single centre, phase Ⅲ, non-inferiority trial[J]. Eur J Surg Oncol EJSO, 2017, 43(4): 672-679. |
| [17] |
KIM B K, PARK B W, HUR M H, et al. Omission of axillary lymph node dissection in patients who underwent total mastectomy with 1 or 2 metastatic lymph nodes[J]. Ann Surg Treat Res, 2020, 98(6): 283-290.
doi: 10.4174/astr.2020.98.6.283 pmid: 32528907 |
| [18] | GAO W Q, LU S S, ZENG Y F, et al. Axilla lymph node dissection can be safely omitted in patients with 1-2 positive sentinel nodes receiving mastectomy: a large multi-institutional study and a systemic meta-analysis[J]. Breast Cancer Res Treat, 2022, 196(1): 129-141. |
| [19] |
FITZSULLIVAN E, BASSETT R L, KUERER H M, et al. Outcomes of sentinel lymph node-positive breast cancer patients treated with mastectomy without axillary therapy[J]. Ann Surg Oncol, 2017, 24(3): 652-659.
doi: 10.1245/s10434-016-5605-5 pmid: 27822630 |
| [20] | TINTERRI C, GENTILE D, GATZEMEIER W, et al. Preservation of axillary lymph nodes compared with complete dissection in T1-2 breast cancer patients presenting one or two metastatic sentinel lymph nodes: the SINODAR-ONE multicenter randomized clinical trial[J]. Ann Surg Oncol, 2022, 29(9): 5732-5744. |
| [21] | GOYAL A, BRUCE MANN G, FALLOWFIELD L, et al. POSNOC-positive sentinel node: adjuvant therapy alone versus adjuvant therapy plus clearance or axillary radiotherapy: a randomised controlled trial of axillary treatment in women with early-stage breast cancer who have metastases in one or two sentinel nodes[J]. BMJ Open, 2021, 11(12): e054365. |
| [22] | WHELAN T J, OLIVOTTO I A, PARULEKAR W R, et al. Regional nodal irradiation in early-stage breast cancer[J]. N Engl J Med, 2015, 373(4): 307-316. |
| [23] | POORTMANS P M, WELTENS C, FORTPIED C, et al. Internal mammary and medial supraclavicular lymph node chain irradiation in stage Ⅰ-Ⅲ breast cancer (EORTC 22922/10925): 15-year results of a randomised, phase 3 trial[J]. Lancet Oncol, 2020, 21(12): 1602-1610. |
| [24] | EBCTCG (Early Breast Cancer Trialists' Collaborative Group). Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8 135 women in 22 randomised trials[J]. Lancet, 2014, 383(9935): 2127-2135. |
| [25] | ALKNER S, DE BONIFACE J, LUNDSTEDT D, et al. Protocol for the T-REX-trial: tailored regional external beam radiotherapy in clinically node-negative breast cancer patients with 1-2 sentinel node macrometastases-an open, multicentre, randomised non-inferiority phase 3 trial[J]. BMJ Open, 2023, 13(9): e075543. |
| [26] | SIT D, LALANI N, CHAN E, et al. Association between regional nodal irradiation and breast cancer recurrence-free interval for patients with low-risk, node-positive breast cancer[J]. Int J Radiat Oncol Biol Phys, 2022, 112(4): 861-869. |
| [27] | 焦得闯, 朱久俊, 乔江华, 等. 前哨淋巴结1-2枚转移的早期乳腺癌患者非前哨淋巴结转移状态分析[J]. 中华普通外科杂志, 2018, 33(7): 571-574. |
| JIAO D C, ZHU J J, QIAO J H, et al. Nonsentinel lymph nodal status in 1-2 sentinel lymph node positive early breast cancer patients[J]. Chin J Gen Surg, 2018, 33(7): 571-574. | |
| [28] |
YANG Z B, LAN X W, HUANG Z, et al. Development and external validation of a nomogram to predict four or more positive nodes in breast cancer patients with one to three positive sentinel lymph nodes[J]. Breast, 2020, 53: 143-151.
doi: S0960-9776(20)30154-5 pmid: 32823167 |
| [29] |
SPECHT M C, KATTAN M W, GONEN M, et al. Predicting nonsentinel node status after positive sentinel lymph biopsy for breast cancer: clinicians versus nomogram[J]. Ann Surg Oncol, 2005, 12(8): 654-659.
pmid: 16021535 |
| [30] |
VAN ZEE K J, MANASSEH D E, BEVILACQUA J L B, et al. A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy[J]. Ann Surg Oncol, 2003, 10(10): 1140-1151.
doi: 10.1245/aso.2003.03.015 pmid: 14654469 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
