Welcome to China Oncology,
China Oncology ›› 2025, Vol. 35 ›› Issue (4): 394-403.doi: 10.19401/j.cnki.1007-3639.2025.04.007
• Article • Previous Articles Next Articles
JIA Ruijie1,2( ), SHI Zhiqiang1,3, ZHANG Qi1, LU Yongjin1,2, ZHENG Junsheng1,2, SUN Jing1,2, BI Zhao1, SUN Xiao1, WANG Yongsheng1, QIU Pengfei1,2(
), SHI Zhiqiang1,3, ZHANG Qi1, LU Yongjin1,2, ZHENG Junsheng1,2, SUN Jing1,2, BI Zhao1, SUN Xiao1, WANG Yongsheng1, QIU Pengfei1,2( )
)
Received:2025-01-06
Revised:2025-03-20
Online:2025-04-30
Published:2025-05-16
Contact:
QIU Pengfei
Supported by:Share article
JIA Ruijie, SHI Zhiqiang, ZHANG Qi, LU Yongjin, ZHENG Junsheng, SUN Jing, BI Zhao, SUN Xiao, WANG Yongsheng, QIU Pengfei. Research on the association of breast cancer patients’ prognosis with internal mammary sentinel lymph node biopsy[J]. China Oncology, 2025, 35(4): 394-403.
Tab. 1
Baseline characteristics of patients before and after propensity score matching (PSM) [n (%)]"
| Characteristic | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
| IMSLNB (n=335) | No-IMSLNB (n=1215) | P value | IMSLNB (n=330) | No-IMSLNB (n=660) | P value | |
| Median age/year | 49.0 | 50.0 | NA | 49.0 | 49.0 | NA |
| Age IQR (Q1-Q3)/year | 42.5-56.0 | 44.0-58.0 | NA | 43.0-56.3 | 43.0-56.0 | NA |
| Age/year | 0.329 | 0.787 | ||||
| ≤50 | 178 (53.1) | 609 (50.1) | 175 (53.0) | 344 (52.1) | ||
| >50 | 157 (46.9) | 606 (49.9) | 155 (47.0) | 316 (47.9) | ||
| Laterality | 0.515 | 0.928 | ||||
| Left | 184 (54.9) | 643 (53.0) | 182 (55.2) | 366 (55.5) | ||
| Right | 151 (45.1) | 572 (47.0) | 148 (44.8) | 294 (44.5) | ||
| Location | <0.001 | 0.322 | ||||
| Outside | 183 (54.6) | 805 (66.3) | 178 (53.9) | 389 (59.0) | ||
| Central/inside | 150 (45.1) | 402 (33.1) | 150 (45.4) | 267 (40.4) | ||
| Multiple/latent | 2 (0.6) | 8 (0.6) | 2 (0.7) | 4 (0.6) | ||
| Histopathologic type | <0.001 | 0.608 | ||||
| Ductal | 296 (88.8) | 946 (77.9) | 293 (88.8) | 593 (89.8) | ||
| Other | 39 (11.2) | 269 (22.1) | 37 (11.2) | 67 (10.2) | ||
| BMI/(kd·m-2) | 0.002 | 0.553 | ||||
| ≤24 | 198 (58.8) | 599 (41.3) | 194 (58.8) | 364 (55.2) | ||
| 24-28 | 106 (31.8) | 427 (35.1) | 105 (31.8) | 229 (34.7) | ||
| ≥28 | 31 (9.4) | 189 (15.5) | 31 (9.4) | 67 (10.1) | ||
| Menopause | 0.117 | 0.413 | ||||
| Yes | 135 (40.3) | 548 (45.1) | 134 (40.6) | 286 (43.3) | ||
| No | 200 (59.7) | 667 (54.9) | 196 (59.4) | 374 (56.7) | ||
| LVI | 0.02 | 0.502 | ||||
| Yes | 90 (26.9) | 255 (21.0) | 88 (26.7) | 163 (24.7) | ||
| No | 245 (73.1) | 960 (79.0) | 242 (73.3) | 497 (75.3) | ||
| Subtype | 0.001 | 0.901 | ||||
| HR+/HER2- | 266 (79.4) | 1 062 (87.4) | 261 (79.1) | 530 (80.3) | ||
| HER2+ | 36 (10.7) | 80 (6.6) | 36 (10.9) | 67 (10.2) | ||
| TNBC | 33 (9.9) | 73 (6.0) | 33 (10.0) | 63 (9.5) | ||
| pT | 0.143 | 0.360 | ||||
| T1 | 179 (53.6) | 725 (59.7) | 177 (53.6) | 385 (58.3) | ||
| T2 | 148 (43.9) | 464 (38.2) | 145 (43.9) | 259 (39.2) | ||
| T3 | 8 (2.4) | 26 (2.1) | 8 (2.4) | 16 (2.4) | ||
| ALN status | 0.025 | 0.371 | ||||
| N0 | 174 (51.2) | 753 (62.0) | 174 (52.7) | 367 (55.6) | ||
| N1 | 85 (25.4) | 290 (23.9) | 83 (25.2) | 152 (23.0) | ||
| N2 | 40 (11.9) | 86 (7.1) | 38 (11.5) | 70 (10.6) | ||
| N3 | 36 (10.7) | 86 (7.1) | 35 (10.6) | 71 (10.8) | ||
Tab. 2
Comparison of IMLN-RT data between two groups"
| ALN status | IMSLNB group | No-IMSLNB group | P value | ||
|---|---|---|---|---|---|
| Patients n | Received IMLN-RT n(%) | Patients n | Received IMLN-RT n(%) | ||
| N0 | 174 | 7 (4.0) | 391 | 0 (0.0) | <0.001 |
| N1 | 83 | 13 (15.7) | 152 | 31 (15.5) | 0.374 |
| N2 | 38 | 20 (52.6) | 70 | 45 (64.3) | 0.241 |
| N3 | 35 | 14 (40.0) | 71 | 48 (67.6) | 0.007 |
| ALN total | 330 | 54 (16.4) | 660 | 124 (18.8) | 0.349 |

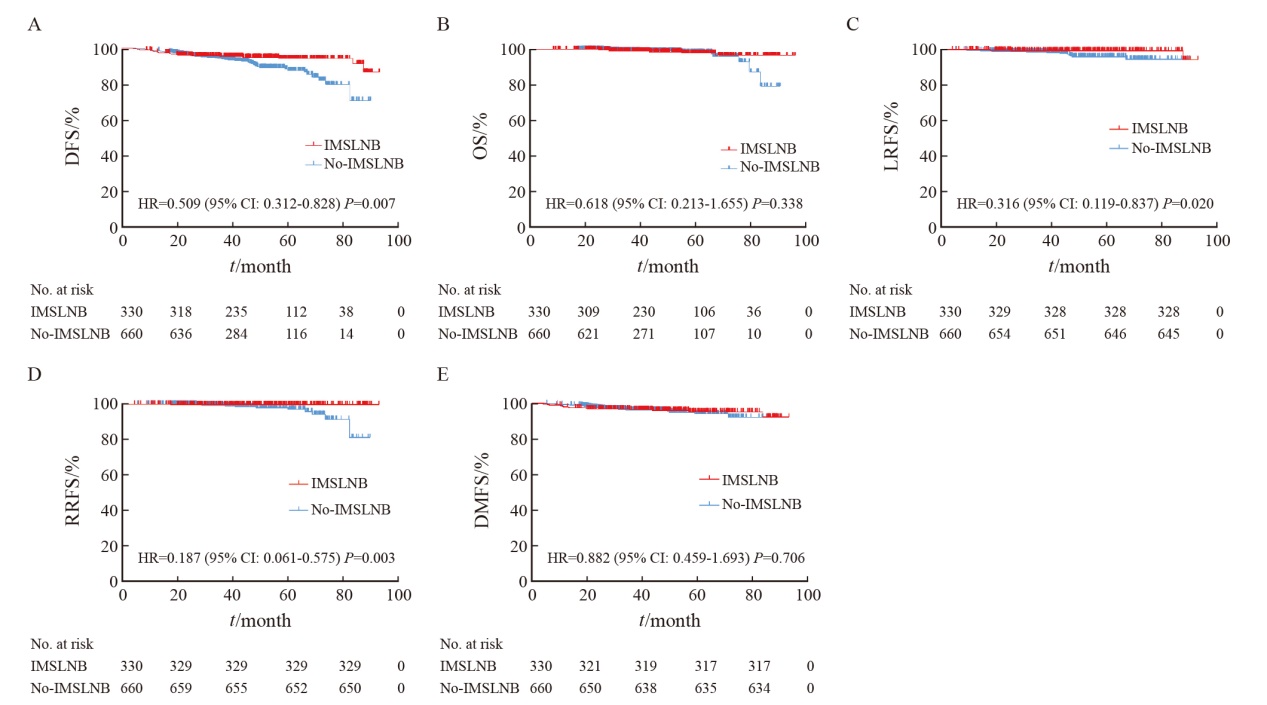
Fig. 2
Kaplan-Meier survival curve analysis Propensity score matching Kaplan-Meier survival analysis showed that there were significant differences in disease-free survival (DFS) and regional relapse-free survival (RFS) between IMSLNB group and No-IMSLNB group, and no significant differences in overall survival (OS), local relapse-free survival (LRFS) and distant metastasis-free survival (DMFS). A: DFS; B: OS; C: LRFS; D: RRFS; E: DMFS."
Tab. 3
Univariate and multivariate Cox analysis of DFS in patients after operation"
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Group | ||||
| No-IMSLNB | 1 | 1 | ||
| IMSLNB | 0.509 (0.312-0.828) | 0.007 | 0.439 (0.245-0.785) | 0.006 |
| Age/year | ||||
| ≤50 | 1 | |||
| >50 | 1.105 (0.693-1.762) | 0.675 | ||
| Menopause | ||||
| No | 1 | |||
| Yes | 1.372 (0.859-2.189) | 0.185 | ||
| BMI/(kg·m-2) | ||||
| ≤24 | 1 | |||
| 24-28 | 0.974 (0.595-1.595) | 0.916 | ||
| ≥28 | 0.467 (0.126-1.312) | 0.132 | ||
| LVI | ||||
| No | 1 | 1 | ||
| Yes | 1.392 (1.189-3.138) | 0.008 | 0.981 (0.586-1.641) | 0.941 |
| Laterality | ||||
| Left | 1 | |||
| Right | 0.954 (0.635-1.618) | 0.954 | ||
| Location | ||||
| Outside | 1 | |||
| Central/medial | 0.930 (0.578-1.496) | 0.764 | ||
| Multiple/latent | 1.717 (0.234-12.578) | 0.595 | ||
| Histopathologic type | ||||
| Ductal | 1 | |||
| Other | 1.427 (0.730-2.791) | 0.298 | ||
| Subtype | ||||
| HR+/HER2- | 1 | 1 | ||
| HER2+ | 1.977 (1.049-3.726) | 0.035 | 2.425 (1.280-4.595) | 0.007 |
| TNBC | 2.168 (1.124-4.182) | 0.021 | 2.102 (1.082-4.081) | 0.028 |
| pT | ||||
| T1 | 1 | 1 | ||
| T2 | 1.357 (0.838-2.199) | 0.215 | 0.796 (0.482-1.313) | 0.371 |
| T3 | 4.688 (1.822-12.063) | 0.001 | 2.079 (0.780-5.540) | 0.143 |
| ALN status | ||||
| N0 | 1 | 1 | ||
| N1 | 4.239 (2.109-8.521) | <0.001 | 4.905 (2.402-10.018) | <0.001 |
| N2 | 9.144 (4.429-18.880) | <0.001 | 13.085 (5.642-30.348) | <0.001 |
| N3 | 8.409 (4.010-17.635) | <0.001 | 9.940 (4.501-21.950) | <0.001 |

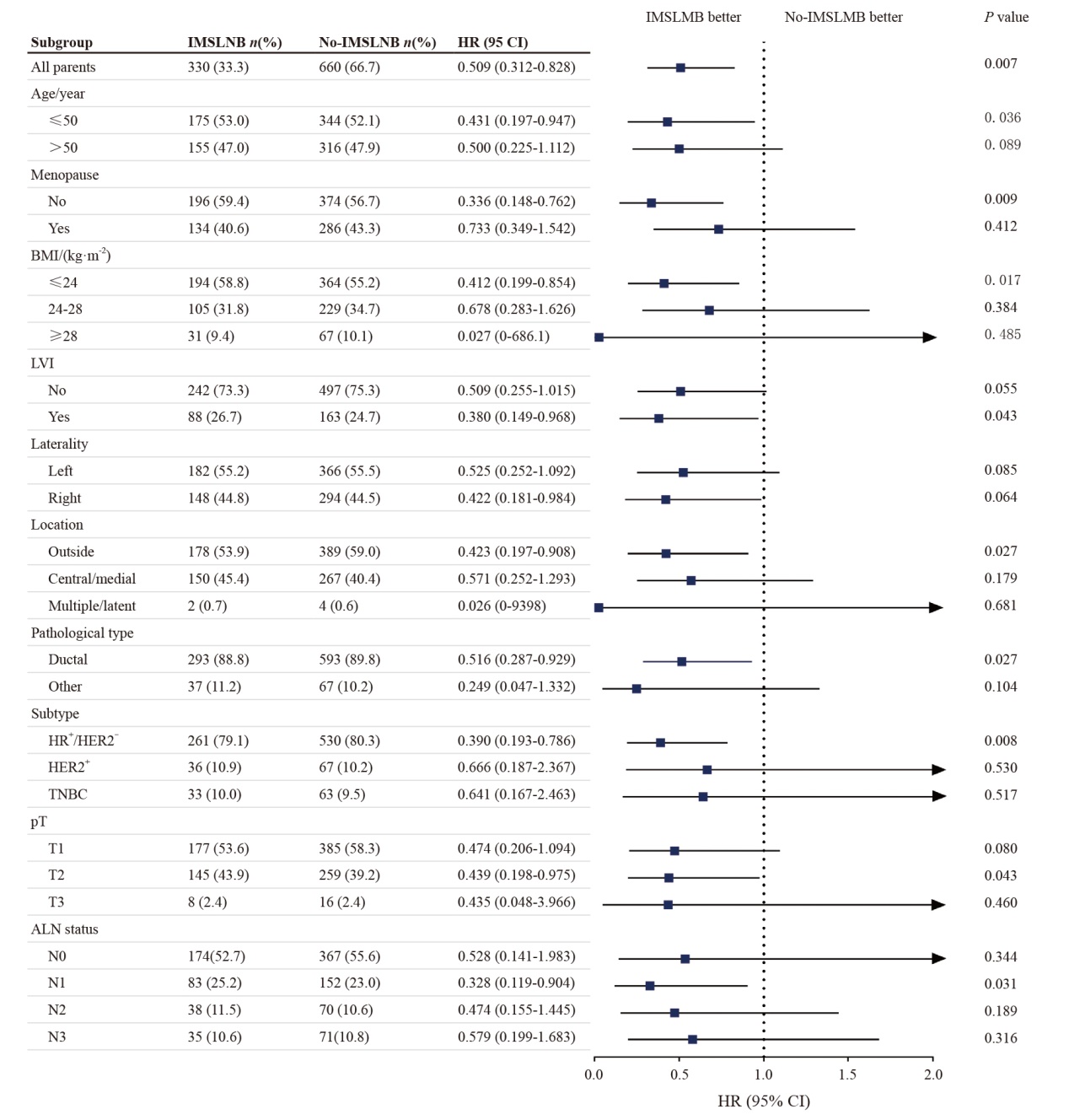
Fig. 3
Forest plot for subgroup analysis of DFS IMSLNB: Internal mammary sentinel lymph node biopsy; BMI: Body mass index; LVI: Lymphatic vessel infiltration; HR+: Hormone receptor positive; HER2: Human epidermal growth factor receptor 2; TNBC: Triple-negative breast cancer; ALN: Axillary lymph node."
Tab. 4
Clinical study on prognosis of IMLN radiotherapy"
| Clinical trial | EORTC 22922/10925 | MA.20 | DBCG-IMN |
|---|---|---|---|
| Enrollment n | 4 004 | 1 832 | 3 089 |
| ALN positive rate | |||
| 0 | 44% | 10% | 0% |
| 1-3 | 43% | 85% | 60% |
| >3 | 13% | 5% | 40% |
| Group | IM-MS RT vs No-IM-MS RT | RNI vs No-RNI | IMNI (right) vs no-IMNI (left) |
| Follow-up t/year | 15.7 | 10 | 15 |
| Result | OS (73.1% vs 70.9%, P=0.36); DFS (60.8% vs 59.9%, P=0.18); DMFS (70.0% vs 68.2%, P=0.18); Mortality (16.0% vs 19.8%, P=0.006) | OS (82.8% vs 81.8%, P=0.38); DFS (82.0% vs 77.0%, P=0.001); DMFS (86.3% vs 82.45, P=0.03) | OS (60.1% vs 55.4%, P=0.007); DMFS (35.6% vs 38.6%, P=0.04); Mortality (31.7% vs33.9%, P=0.05) |
| [1] | BRAY F, LAVERSANNE M, SUNG H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2024, 74(3): 229-263. |
| [2] |
JOO J H, KIM S S, SON B H, et al. Evaluation of the prognostic stage in the 8th edition of the American Joint Committee on cancer in patients with breast cancer and internal mammary lymph node metastasis[J]. Anticancer Res, 2018, 38(9): 5357-5361.
doi: 10.21873/anticanres.12864 pmid: 30194189 |
| [3] |
VERONESI U, MARUBINI E, MARIANI L, et al. The dissection of internal mammary nodes does not improve the survival of breast cancer patients. 30-year results of a randomised trial[J]. Eur J Cancer, 1999, 35(9): 1320-1325.
doi: 10.1016/s0959-8049(99)00133-1 pmid: 10658521 |
| [4] |
MANCA G, TARDELLI E, RUBELLO D, et al. Sentinel lymph node biopsy in breast cancer: a technical and clinical appraisal[J]. Nucl Med Commun, 2016, 37(6): 570-576.
doi: 10.1097/MNM.0000000000000489 pmid: 26886421 |
| [5] |
LYMAN G H, SOMERFIELD M R, BOSSERMAN L D, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update[J]. J Clin Oncol, 2017, 35(5): 561-564.
doi: 10.1200/JCO.2016.71.0947 pmid: 27937089 |
| [6] |
邱鹏飞, 王永胜. 前哨淋巴结时代乳腺癌的精准区域处理: 演进与展望[J]. 中国癌症杂志, 2022, 32(8): 680-687.
doi: 10.19401/j.cnki.1007-3639.2022.08.002 |
| QIU P F, WANG Y S. Precise regional management of breast cancer in the sentinel lymph node era: evolution and prospect[J]. China Oncol, 2022, 32(8): 680-687. | |
| [7] |
GNERLICH J L, CAMILO BARRETO-ANDRADE J, CZECHURA T, et al. Accurate staging with internal mammary chain sentinel node biopsy for breast cancer[J]. Ann Surg Oncol, 2014, 21(2): 368-374.
doi: 10.1245/s10434-013-3263-4 pmid: 24046119 |
| [8] | CONG B B, QIU P F, WANG Y S. Internal mammary sentinel lymph node biopsy: minimally invasive staging and tailored internal mammary radiotherapy[J]. Ann Surg Oncol, 2014, 21(7): 2119-2121. |
| [9] | QIU P F, ZHAO R R, WANG W, et al. Internal mammary sentinel lymph node biopsy in clinically axillary lymph node-positive breast cancer: diagnosis and implications for patient management[J]. Ann Surg Oncol, 2020, 27(2): 375-383. |
| [10] | WANG K, ZHANG X, ZHENG K, et al. Predictors of internal mammary lymph nodes (IMLN) metastasis and disease-free survival comparison between IMLN-positive and IMLN-negative breast cancer patients: results from Western China Clinical Cooperation Group (WCCCG) database (CONSORT)[J]. Medicine (Baltimore), 2018, 97(28): e11296. |
| [11] | GRADISHAR W J, ANDERSON B O, BALASSANIAN R, et al. NCCN guidelines insights breast cancer, version 1.2016[J]. J Natl Compr Canc Netw, 2015, 13(12): 1475-1485. |
| [12] | QIU P F, CONG B B, ZHAO R R, et al. Internal mammary sentinel lymph node biopsy with modified injection technique: high visualization rate and accurate staging[J]. Medicine (Baltimore), 2015, 94(41): e1790. |
| [13] | QIU P F, LV Q, ZHAO W H, et al. Development and validation of a nomogram for predicting internal mammary sentinel node metastasis in breast cancer patients[J]. Eur J Surg Oncol, 2023, 49(10): 107040. |
| [14] | WANG Y S, LV Q, ZHU SG, et al. Prospective, multicenter, clinical validation study of internal mammary sentinel lymph node biopsy followed by internal mammary lymph node dissection with the modified injection technique (CBCSG026/27)[C]. SABCS19-P1-20-14. |
| [15] | POORTMANS P M, WELTENS C, FORTPIED C, et al. Internal mammary and medial supraclavicular lymph node chain irradiation in stage Ⅰ-Ⅲ breast cancer (EORTC 22922/10925): 15-year results of a randomised, phase 3 trial[J]. Lancet Oncol, 2020, 21(12): 1602-1610. |
| [16] | WHELAN T J, OLIVOTTO I A, PARULEKAR W R, et al. Regional nodal irradiation in early-stage breast cancer[J]. N Engl J Med, 2015, 373(4): 307-316. |
| [17] | THORSEN L B J, OVERGAARD J, MATTHIESSEN L W, et al. Internal mammary node irradiation in patients with node-positive early breast cancer: fifteen-year results from the Danish breast cancer group internal mammary node study[J]. J Clin Oncol, 2022, 40(36): 4198-4206. |
| [18] | CONG B B, CAO X S, CAO L, et al. Internal mammary lymph nodes radiotherapy of breast cancer in the era of individualized medicine[J]. Oncotarget, 2017, 8(46): 81583-81590. |
| [19] |
陈玉光, 孙晓, 毕钊, 等. 乳腺癌内乳前哨淋巴结活检评估预后及指导个体化内乳照射: 一项长期随访研究[J]. 中国癌症杂志, 2023, 33(2): 142-151.
doi: 10.19401/j.cnki.1007-3639.2023.02.007 |
| CHEN Y G, SUN X, BI Z, et al. Internal mammary sentinel lymph node biopsy for breast cancer: a long-term follow-up research for assessment of prognosis and guiding individualized internal mammary lymph node irradiation[J]. China Oncol, 2023, 33(2): 142-151. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
