Welcome to China Oncology,
China Oncology ›› 2025, Vol. 35 ›› Issue (8): 752-760.doi: 10.19401/j.cnki.1007-3639.2025.08.003
• Article • Previous Articles Next Articles
WANG Mengxiao1( ), FAN Wendong2(
), FAN Wendong2( ), CAO Jingjing1, CHEN Jiayi1,2, CAI Gang2(
), CAO Jingjing1, CHEN Jiayi1,2, CAI Gang2( ), CAO Lu1(
), CAO Lu1( )
)
Received:2025-03-04
Revised:2025-06-05
Online:2025-08-30
Published:2025-09-10
Contact:
CAI Gang, CAO Lu
Supported by:Share article
CLC Number:
WANG Mengxiao, FAN Wendong, CAO Jingjing, CHEN Jiayi, CAI Gang, CAO Lu. Set-up error and CTV margin in one-week ultra-hypofractionated whole breast irradiation after breast-conserving surgery based on daily CBCT[J]. China Oncology, 2025, 35(8): 752-760.
Tab. 1
Clinicopathological characteristics of the patients"
| Characteristics | Patients (n=34) |
|---|---|
| Age median (range)/year | 53.5 (40.0, 74.0) |
| CTV volume median (range)/cm3 | 402.5 (143.2, 958.6) |
| Height median (range)/cm | 161.5 (150.0, 168.0) |
| Weight median (range)/kg | 60.0 (45.0, 78.0) |
| BMI median (range)/ (kg·m-2) | 23.2 (18.0, 28.0) |
| Laterality n(%) | |
| Left | 22 (64.7) |
| Right | 12 (35.3) |
| Quadrant n(%) | |
| Upper inner | 6 (17.6) |
| Lower inner | 4 (11.8) |
| Upper outer | 20 (58.8) |
| Lower outer | 4 (11.8) |
| Axillary surgery n(%) | |
| Sentinel lymph node biopsy | 32 (94.1) |
| None | 2 (5.9) |
| Pathological tumor stage n(%) | |
| pTis | 6 (17.6) |
| pT1 | 24 (70.6) |
| pT2 | 4 (11.8) |
| Pathological nodal stage n(%) | |
| pNx | 2 (5.9) |
| pN0 | 31 (91.2) |
| pN1mi | 1 (2.9) |
| Subtype n(%) | |
| HR+/HER2+ | 2 (5.9) |
| HR+/HER2- | 27 (79.4) |
| HR-/HER2+ | 1 (2.9) |
| HR-/HER2- | 4 (11.8) |
| Adjuvant therapy n(%) | |
| None | 19 (55.8) |
| Chemotherapy | 12 (35.3) |
| Chemotherapy+anti-HER2 therapy | 3 (8.8) |

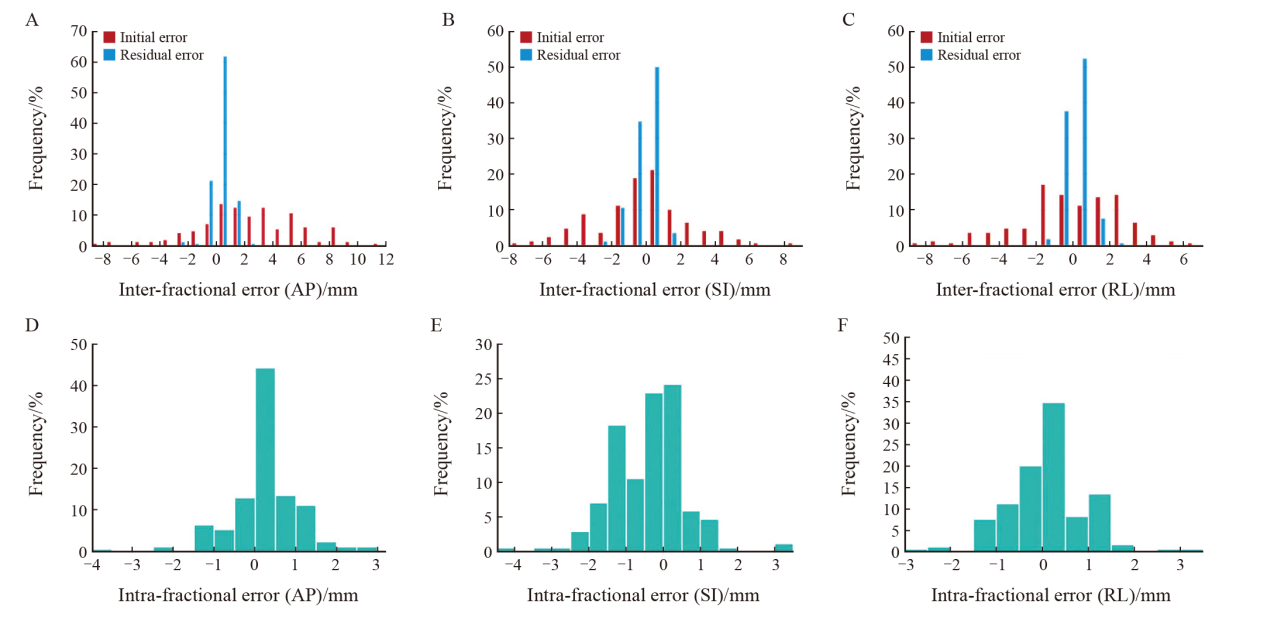
Fig. 4
Distributions of inter-fractional and intra-fractional errors of 170 fractions in overall cohort A-C: Distributions of initial and residual inter-fractional errors in anterior-posterior (AP), superior-inferior (SI) and right-left (RL) directions. D-F: Distributions of intra-fractional errors in AP, SI or RL directions."
Tab. 2
Comparison of residual inter-fractional error between patients with different clinical characteristics."
| AP/mm | SI/mm | RL/mm | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (range) | Z valuea/ H valueb | P value | Median (range) | Z value/ H value | P value | Median (range) | Z value/ H value | P value | |||
| Age/year | -0.818 | 0.414 | -0.335 | 0.738 | -0.003 | 0.997 | |||||
| ≤53.5 | 0.5 (0.0, 2.1) | 0.5 (0.0, 2.1) | 0.3 (0.0, 2.6) | ||||||||
| >53.5 | 0.4 (0.0, 2.4) | 0.5 (0.2, 2.0) | 0.3 (0.0, 1.9) | ||||||||
| CTV/cm3 | -2.265 | 0.023 | -2.083 | 0.037 | -1.587 | 0.112 | |||||
| ≤402.5 | 0.3 (0.0, 2.4) | 0.5 (0.0, 2.0) | 0.4 (0.0, 2.6) | ||||||||
| >402.5 | 0.5 (0.0, 2.1) | 0.6 (0.0, 2.1) | 0.2 (0.0, 1.9) | ||||||||
| Height/cm | -2.206 | 0.027 | -0.770 | 0.441 | -0.480 | 0.631 | |||||
| ≤161.5 | 0.4 (0.0, 2.1) | 0.5 (0.0, 2.1) | 0.2 (0.0, 2.6) | ||||||||
| >161.5 | 0.4 (0.0, 2.4) | 0.5 (0.0, 2.0) | 0.3 (0.0, 1.9) | ||||||||
| Weight/kg | -0.839 | 0.401 | -0.804 | 0.421 | -0.710 | 0.478 | |||||
| ≤60.0 | 0.4 (0.0, 2.4) | 0.5 (0.0, 2.1) | 0.4 (0.0, 2.6) | ||||||||
| >60.0 | 0.5 (0.0, 2.1) | 0.5 (0.0, 1.9) | 0.2 (0.0, 1.9) | ||||||||
| BMI/(kg·m-2) | -0.252 | 0.801 | -1.701 | 0.089 | -0.848 | 0.396 | |||||
| ≤23.2 | 0.4 (0.0, 2.4) | 0.5 (0.0, 2.0) | 0.4 (0.0, 2.6) | ||||||||
| >23.2 | 0.4 (0.0, 2.1) | 0.5 (0.0, 2.1) | 0.3 (0.0, 1.9) | ||||||||
| Laterality | -0.987 | 0.324 | -1.299 | 0.194 | -1.520 | 0.129 | |||||
| Left | 0.4 (0.0, 2.1) | 0.5 (0.0, 1.9) | 0.3 (0.0, 2.6) | ||||||||
| Right | 0.6 (0.0, 2.4) | 0.5 (0.1, 2.1) | 0.4 (0.0, 1.9) | ||||||||
| Quadrant | 1.862 | 0.601 | 7.222 | 0.065 | 2.754 | 0.431 | |||||
| Upper inner | 0.5 (0.0, 2.4) | 0.5 (0.0, 2.0) | 0.4 (0.0, 2.6) | ||||||||
| Lower inner | 0.5 (0.0, 1.3) | 0.8 (0.1, 1.8) | 0.2 (0.0, 0.9) | ||||||||
| Upper outer | 0.4 (0.0, 2.1) | 0.5 (0.0, 2.1) | 0.4 (0.0, 1.9) | ||||||||
| Lower outer | 0.4 (0.1, 2.1) | 0.8 (0.0, 1.9) | 0.3 (0.0, 1.0) | ||||||||
| Adjuvant therapy | -1.495 | 0.135 | -1.414 | 0.157 | -0.370 | 0.711 | |||||
| None | 0.4 (0.0, 2.1) | 0.5 (0.0, 2.1) | 0.3 (0.0, 2.6) | ||||||||
| Yes | 0.5 (0.0, 2.4) | 0.6 (0.0, 2.0) | 0.3 (0.0, 1.4) | ||||||||
Tab. 3
Comparison of intra-fractional error between patients with different clinical characteristics"
| Item | AP/mm | SI/mm | RL/mm | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (range) | Z valuea/ H valueb | P value | Median (range) | Z value/ H value | P value | Median (range) | Z value/ H value | P value | |||
| Age/year | -1.109 | 0.267 | -0.713 | 0.476 | -0.743 | 0.457 | |||||
| ≤53.5 | 0.2 (0.0, 3.9) | 0.8 (0.0, 4.4) | 0.5 (0.0, 3.1) | ||||||||
| >53.5 | 0.4 (0.0, 2.6) | 0.6 (0.0, 3.0) | 0.2 (0.0, 2.8) | ||||||||
| CTV/cm3 | -3.308 | 0.001 | -1.286 | 0.198 | -1.156 | 0.248 | |||||
| ≤402.5 | 0.2 (0.0, 2.4) | 0.5 (0.0, 4.4) | 0.2 (0.0, 3.1) | ||||||||
| >402.5 | 0.5 (0.0, 3.9) | 0.9 (0.0, 3.5) | 0.4 (0.0, 2.5) | ||||||||
| Height/cm | -1.329 | 0.184 | -0.347 | 0.729 | -0.555 | 0.579 | |||||
| ≤161.5 | 0.2 (0.0, 3.9) | 0.6 (0.0, 4.4) | 0.3 (0.0, 3.1) | ||||||||
| >161.5 | 0.4 (0.0, 2.6) | 0.7 (0.0, 3.5) | 0.3 (0.0, 2.2) | ||||||||
| Weight/kg | -2.129 | 0.033 | -0.461 | 0.645 | -0.597 | 0.550 | |||||
| ≤60.0 | 0.2 (0.0, 3.9) | 0.7 (0.0, 4.4) | 0.3 (0.0, 3.1) | ||||||||
| >60.0 | 0.5 (0.0, 2.6) | 0.6 (0.0, 3.5) | 0.5 (0.0, 1.9) | ||||||||
| BMI/(kg·m-2) | -3.506 | <0.001 | -1.624 | 0.104 | -1.501 | 0.133 | |||||
| ≤23.2 | 0.2 (0.0, 2.3) | 0.5 (0.0, 3.5) | 0.3 (0.0, 3.1) | ||||||||
| >23.2 | 0.7 (0.0, 3.9) | 0.8 (0.0, 4.4) | 0.5 (0.0, 2.5) | ||||||||
| Laterality | -0.350 | 0.726 | -1.571 | 0.116 | -1.692 | 0.091 | |||||
| Left | 0.3 (0.0, 2.5) | 0.6 (0.0, 3.0) | 0.6 (0.0, 3.1) | ||||||||
| Right | 0.3 (0.0, 3.9) | 0.9 (0.0, 4.4) | 0.2 (0.0, 2.8) | ||||||||
| Quadrant | 1.336 | 0.721 | 10.375 | 0.016 | 7.106 | 0.069 | |||||
| Upper inner | 0.2 (0.0, 1.1) | 0.3 (0.0, 2.4) | 0.2 (0.0, 2.2) | ||||||||
| Lower inner | 0.2 (0.0, 2.4) | 1.3 (0.0, 4.4) | 0.3 (0.0, 1.5) | ||||||||
| Upper outer | 0.3 (0.0, 3.9) | 0.5 (0.0, 3.0) | 0.5 (0.0, 3.1) | ||||||||
| Lower outer | 0.3 (0.0, 2.2) | 0.9 (0.0, 3.0) | 0.9 (0.0, 1.9) | ||||||||
| Adjuvant therapy | -0.297 | 0.766 | -1.841 | 0.066 | -0.224 | 0.823 | |||||
| None | 0.2 (0.0, 3.9) | 0.8 (0.0, 4.4) | 0.3 (0.0, 3.1) | ||||||||
| Yes | 0.4 (0.0, 2.3) | 0.3 (0.0, 3.5) | 0.3 (0.0, 2.2) | ||||||||
Tab. 4
CTV to PTV margin in single-week ultra-hypofractionated whole breast irradiation"
| Item | Margin without daily CBCT/mm | Margin with daily CBCT/mm | |||||
|---|---|---|---|---|---|---|---|
| AP | SI | RL | AP | SI | RL | ||
| Overall cohort (n=34) | 8.9 | 7.2 | 7.1 | 2.3 | 2.8 | 2.0 | |
| Categorized by BMI | |||||||
| ≤23.2kg/m2 (n=17) | 9.0 | 6.3 | 5.6 | 1.8 | 2.3 | 2.0 | |
| >23.2kg/m2 (n=17) | 8.6 | 7.9 | 8.4 | 2.6 | 3.4 | 2.0 | |
| Categorized by height | |||||||
| ≤161.5 cm (n=17) | 8.6 | 4.6 | 6.8 | 2.2 | 2.7 | 2.3 | |
| >161.5 cm (n=17) | 9.2 | 8.6 | 7.5 | 2.3 | 2.9 | 1.8 | |
| Categorized by weight | |||||||
| ≤60.0 kg (n=19) | 8.7 | 6.2 | 6.0 | 2.2 | 2.7 | 2.2 | |
| >60.0 kg (n=15) | 9.2 | 8.2 | 8.2 | 2.4 | 2.9 | 1.7 | |
| Categorized by CTV | |||||||
| ≤402.5 cm3 (n=17) | 6.8 | 6.4 | 5.9 | 1.6 | 2.6 | 2.1 | |
| >402.5 cm3 (n=17) | 10.1 | 8.0 | 8.2 | 2.8 | 3.1 | 2.0 | |
| Categorized by quadrant | |||||||
| Upper inner quadrant (n=6) | 6.5 | 5.5 | 5.1 | 1.8 | 2.2 | 2.0 | |
| Lower inner quadrant (n=4) | 10.7 | 5.8 | 4.5 | 1.8 | 2.5 | 1.8 | |
| Upper outer quadrant (n=20) | 9.1 | 7.7 | 7.5 | 2.2 | 2.6 | 2.1 | |
| Lower outer quadrant (n=4) | 7.3 | 7.8 | 7.5 | 2.9 | 4.2 | 2.1 | |
| [1] | Early Breast Cancer Trialists; Collaborative Group (EBCTCG), DARBY S, MCGALE P, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials[J]. Lancet, 2011, 378(9804): 1707-1716. |
| [2] |
BRUNT A M, HAVILAND J S, WHEATLEY D A, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial[J]. Lancet, 2020, 395(10237): 1613-1626.
doi: S0140-6736(20)30932-6 pmid: 32580883 |
| [3] | 杨伟志, 冯宁远, 沈瑜. LQ公式的生物学概念及应用[J]. 中华放射肿瘤学杂志, 1995, 4(2): 59-63. |
| YANG W Z, FENG N Y, SHEN Y. Biological concept and application of LQ formula[J]. Chin J Radiat Oncol, 1995, 4(2): 59-63. | |
| [4] |
VAN H M. Errors and margins in radiotherapy[J]. Semin Radiat Oncol, 2004, 14(1): 52-64.
doi: 10.1053/j.semradonc.2003.10.003 pmid: 14752733 |
| [5] |
LEE J, LIU S H, LIN J B, et al. Image-guided study of inter-fraction and intra-fraction set-up variability and margins in reverse semi-decubitus breast radiotherapy[J]. Radiat Oncol, 2018, 13(1): 254.
doi: 10.1186/s13014-018-1200-1 pmid: 30587208 |
| [6] | SIGAUDI V, ZANNETTI M, FERRARA E, et al. Ultra-hypofractionation for whole-breast irradiation in early breast cancer: interim analysis of a prospective study[J]. Biomedicines, 2022, 10(10): 2568. |
| [7] | IVANOV O, MILOVANČEV A, PETROVIĆ B, et al. Ultra-hypofractionated vs moderate fractionated whole breast three dimensional conformal radiotherapy during the COVID-19 pandemic[J]. Medicina (Kaunas), 2022, 58(6): 745. |
| [8] | TOPOLNJAK R, SONKE J J, NIJKAMP J, et al. Breast patient setup error assessment: comparison of electronic portal image devices and cone-beam computed tomography matching results[J]. Int J Radiat Oncol Biol Phys, 2010, 78(4): 1235-1243. |
| [9] |
KEIPER T D, TAI A, CHEN X F, et al. Feasibility of real-time motion tracking using cine MRI during MR-guided radiation therapy for abdominal targets[J]. Med Phys, 2020, 47(8): 3554-3566.
doi: 10.1002/mp.14230 pmid: 32402111 |
| [10] | MALONE C, RYAN S, NICHOLSON J, et al. Intrafraction motion in surface-guided breast radiation therapy and its implications on a single planning target volume margin strategy[J]. Pract Radiat Oncol, 2025, 15(1): e63-e71. |
| [11] | TOKUDA P J K, MITSUYOSHI T, ONO Y, et al. Acute adverse events of ultra-hypofractionated whole-breast irradiation after breast-conserving surgery for early breast cancer in Japan: an interim analysis of the multi-institutional phase Ⅱ UPBEAT study[J]. Breast Cancer, 2024, 31(4): 643-648. |
| [12] |
LUO J R, YIN Z H, ZHANG Z, et al. Does the protocol-required uniform margin around the CTV adequately account for setup inaccuracies in whole breast irradiation?[J]. Radiat Oncol, 2021, 16(1): 143.
doi: 10.1186/s13014-021-01863-w pmid: 34344403 |
| [13] |
HOEKSTRA N, HABRAKEN S, SWAAK-KRAGTEN A, et al. Intrafraction motion during partial breast irradiation depends on treatment time[J]. Radiother Oncol, 2021, 159: 176-182.
doi: 10.1016/j.radonc.2021.03.029 pmid: 33798609 |
| [14] | BODA-HEGGEMANN J, KNOPF A C, SIMEONOVA-CHERGOU A, et al. Deep inspiration breath hold-based radiation therapy: a clinical review[J]. Int J Radiat Oncol Biol Phys, 2016, 94(3): 478-492. |
| [15] | HEIKKILÄ A, BOMAN E, ROSSI M, et al. Dosimetric effect of rotational setup errors in volumetric modulated arc therapy and field-in-field treatment of left-sided breast cancer[J]. Phys Med, 2024, 117: 103203. |
| [16] | LI G. Advances and potential of optical surface imaging in radiotherapy[J]. Phys Med Biol, 2022, 67(16): 10.1088/1361-10.1088/6560/ac838f. |
| [17] |
LIU H F, SCHAAL D, CURRY H, et al. Review of cone beam computed tomography based online adaptive radiotherapy: current trend and future direction[J]. Radiat Oncol, 2023, 18(1): 144.
doi: 10.1186/s13014-023-02340-2 pmid: 37660057 |
| [18] | RIETMAN J S, DIJKSTRA P U, GEERTZEN J B, et al. Treatment-related upper limb morbidity 1 year after sentinel lymph node biopsy or axillary lymph node dissection for stage Ⅰ or Ⅱ breast cancer[J]. Ann Surg Oncol, 2004, 11(11): 1018-1024. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
