Welcome to China Oncology,
China Oncology ›› 2022, Vol. 32 ›› Issue (10): 936-947.doi: 10.19401/j.cnki.1007-3639.2022.10.002
• Specialists'Article • Previous Articles Next Articles
CHEN Yifan1,2,3( ), SHEN Yihui2,3,4, CHENG Leilei2,3,4(
), SHEN Yihui2,3,4, CHENG Leilei2,3,4( ), LIN Jinyi1,2,3, ZHANG Hui2,3,4, WANG Xuejun2,3,4, XU Yuchen1,2,3, ZHANG Jian2,3,4, GE Junbo1,2,3
), LIN Jinyi1,2,3, ZHANG Hui2,3,4, WANG Xuejun2,3,4, XU Yuchen1,2,3, ZHANG Jian2,3,4, GE Junbo1,2,3
Online:2022-10-30
Published:2022-11-29
Share article
CLC Number:
CHEN Yifan, SHEN Yihui, CHENG Leilei, LIN Jinyi, ZHANG Hui, WANG Xuejun, XU Yuchen, ZHANG Jian, GE Junbo. Different preventive effects of four cardioprotective agents on mice with adriamycin-induced cardiotoxicity[J]. China Oncology, 2022, 32(10): 936-947.
Tab. 1
LV functional parameters in doxorubicin-treated mice"
| Item | Saline | Adriamycin | Benazepril | Atorvastatin | Sacubitril/valsartan | Carvedilol |
|---|---|---|---|---|---|---|
| Heart Rate/bpm | 398±48 | 406±59 | 428±66 | 423±79 | 448±59 | 423±55 |
| LVEDD/mm | 3.73±0.31 | 3.78±0.29 | 3.65±0.15 | 3.60±0.28 | 3.40±0.29* | 3.62±0.22 |
| LVESD/mm | 2.44±0.31 | 2.84±0.38# | 2.41±0.18* | 2.41±0.27* | 2.25±0.30* | 2.43±0.23* |
| LVEF/% | 65.7±4.7 | 52.2±5.1# | 63.5±4.6* | 61.6±4.1* | 65.1±3.8* | 62.1±5.2* |
| FS/% | 34.8±4.1 | 26.4±3.1# | 33.9±3.3* | 32.6±2.8* | 34.2±3.7* | 33.0±3.6* |
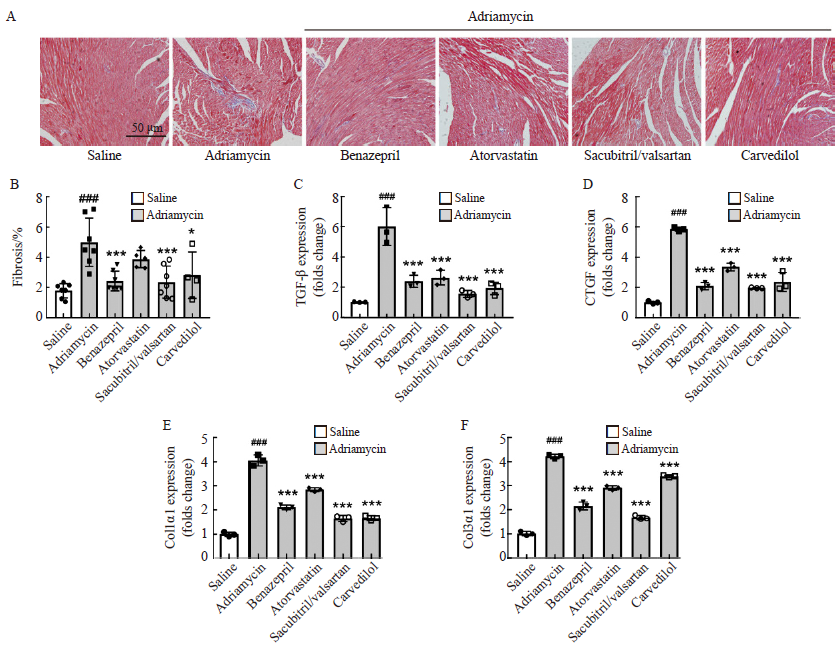
Fig. 2
Effects of four agents on myocardial fibrosis A: Masson’s trichrome staining in Left ventricular (scale bar: 50µm); B: Percentage of myocardial fibrosis; C-F: mRNA levels of profibrotic genes TGF-β, CTGF and Col1α1, and Col3α1). *: P<0.05, **: P<0.01, ***: P<0.001, compared with the adriamycin group; #: P<0.05, ##: P<0.01, ###: P <0.001, compared with the saline group."
| [1] |
Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials[J]. Lancet, 2005, 365(9472): 1687-1717.
doi: 10.1016/S0140-6736(05)66544-0 pmid: 15894097 |
| [2] |
SINGAL P K, ILISKOVIC N. Doxorubicin-induced cardiomyopathy[J]. N Engl J Med, 1998, 339(13): 900-905.
doi: 10.1056/NEJM199809243391307 |
| [3] |
FELKER G M, THOMPSON R E, HARE J M, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy[J]. N Engl J Med, 2000, 342(15): 1077-1084.
doi: 10.1056/NEJM200004133421502 |
| [4] |
MANTAWY E M, EL-BAKLY W M, ESMAT A, et al. Chrysin alleviates acute doxorubicin cardiotoxicity in rats via suppression of oxidative stress, inflammation and apoptosis[J]. Eur J Pharmacol, 2014, 728: 107-118.
doi: 10.1016/j.ejphar.2014.01.065 pmid: 24509133 |
| [5] |
GUO R M, LIN J C, XU W M, et al. Hydrogen sulfide attenuates doxorubicin-induced cardiotoxicity by inhibition of the p38 MAPK pathway in H9c2 cells[J]. Int J Mol Med, 2013, 31(3): 644-650.
doi: 10.3892/ijmm.2013.1246 |
| [6] |
GUO R M, WU K, CHEN J F, et al. Exogenous hydrogen sulfide protects against doxorubicin-induced inflammation and cytotoxicity by inhibiting p38MAPK/NFκB pathway in H9c2 cardiac cells[J]. Cell Physiol Biochem, 2013, 32(6): 1668-1680.
doi: 10.1159/000356602 pmid: 24356372 |
| [7] |
ROCCA C, PASQUA T, CERRA M C, et al. Cardiac damage in anthracyclines therapy: focus on oxidative stress and inflammation[J]. Antioxid Redox Signal, 2020, 32(15): 1081-1097.
doi: 10.1089/ars.2020.8016 |
| [8] |
TIMM K N, TYLER D J. The role of AMPK activation for cardioprotection in doxorubicin-induced cardiotoxicity[J]. Cardiovasc Drugs Ther, 2020, 34(2): 255-269.
doi: 10.1007/s10557-020-06941-x pmid: 32034646 |
| [9] |
CARDINALE D, COLOMBO A, BACCHIANI G, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy[J]. Circulation, 2015, 131(22): 1981-1988.
doi: 10.1161/CIRCULATIONAHA.114.013777 pmid: 25948538 |
| [10] |
ZAMORANO J L, LANCELLOTTI P, RODRIGUEZ MUÑOZ D, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for practice guidelines[J]. Eur J Heart Fail, 2017, 19(1): 9-42.
doi: 10.1002/ejhf.654 |
| [11] |
CHENG J, KAMIYA K, KODAMA I. Carvedilol: molecular and cellular basis for its multifaceted therapeutic potential[J]. Cardiovasc Drug Rev, 2001, 19(2): 152-171.
pmid: 11484068 |
| [12] | DULIN B, ABRAHAM W T. Pharmacology of carvedilol[J]. Am J Cardiol, 2004, 93(9): 3-6. |
| [13] |
GAO G, JIANG S L, GE L L, et al. Atorvastatin improves doxorubicin-induced cardiac dysfunction by modulating Hsp70, Akt, and MAPK signaling pathways[J]. J Cardiovasc Pharmacol, 2019, 73(4): 223-231.
doi: 10.1097/FJC.0000000000000646 pmid: 30540688 |
| [14] |
MCMURRAY J J, PACKER M, DESAI A S, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure[J]. N Engl J Med, 2014, 371(11): 993-1004.
doi: 10.1056/NEJMoa1409077 |
| [15] |
XIA Y, CHEN Z W, CHEN A, et al. LCZ696 improves cardiac function via alleviating Drp1-mediated mitochondrial dysfunction in mice with doxorubicin-induced dilated cardiomyopathy[J]. J Mol Cell Cardiol, 2017, 108: 138-148.
doi: S0022-2828(17)30113-X pmid: 28623750 |
| [16] |
PAN J A, TANG Y, YU J Y, et al. miR-146a attenuates apoptosis and modulates autophagy by targeting TAF9b/P53 pathway in doxorubicin-induced cardiotoxicity[J]. Cell Death Dis, 2019, 10(9): 668.
doi: 10.1038/s41419-019-1901-x |
| [17] |
HULLIN R, MÉTRICH M, SARRE A, et al. Diverging effects of enalapril or eplerenone in primary prevention against doxorubicin-induced cardiotoxicity[J]. Cardiovasc Res, 2018, 114(2): 272-281.
doi: 10.1093/cvr/cvx162 pmid: 29016737 |
| [18] |
MUCHIR A, WU W, SERA F, et al. Mitogen-activated protein kinase kinase 1/2 inhibition and angiotensin Ⅱ converting inhibition in mice with cardiomyopathy caused by lamin A/C gene mutation[J]. Biochem Biophys Res Commun, 2014, 452(4): 958-961.
doi: 10.1016/j.bbrc.2014.09.020 |
| [19] |
ZHAN D Y, MORIMOTO S, DU C K, et al. Therapeutic effect of{beta}-adrenoceptor blockers using a mouse model of dilated cardiomyopathy with a troponin mutation[J]. Cardiovasc Res, 2009, 84(1): 64-71.
doi: 10.1093/cvr/cvp168 |
| [20] |
ZHANG Q L, YANG J J, ZHANG H S. Carvedilol (CAR) combined with carnosic acid (CAA) attenuates doxorubicin-induced cardiotoxicity by suppressing excessive oxidative stress, inflammation, apoptosis and autophagy[J]. Biomed Pharmacother, 2019, 109: 71-83.
doi: 10.1016/j.biopha.2018.07.037 |
| [21] |
YE Y, GONG H, WANG X X, et al. Combination treatment with antihypertensive agents enhances the effect of qiliqiangxin on chronic pressure overload-induced cardiac hypertrophy and remodeling in male mice[J]. J Cardiovasc Pharmacol, 2015, 65(6): 628-639.
doi: 10.1097/FJC.0000000000000230 pmid: 25806688 |
| [22] |
LIPSHULTZ S E, SCULLY R E, LIPSITZ S R, et al. Assessment of dexrazoxane as a cardioprotectant in doxorubicin-treated children with high-risk acute lymphoblastic leukaemia: long-term follow-up of a prospective, randomised, multicentre trial[J]. Lancet Oncol, 2010, 11(10): 950-961.
doi: 10.1016/S1470-2045(10)70204-7 pmid: 20850381 |
| [23] |
LI M C, SALA V, DE SANTIS M C, et al. Phosphoinositide 3-kinase gamma inhibition protects from anthracycline cardiotoxicity and reduces tumor growth[J]. Circulation, 2018, 138(7): 696-711.
doi: 10.1161/CIRCULATIONAHA.117.030352 pmid: 29348263 |
| [24] |
PACKER M, MCMURRAY J J, DESAI A S, et al. Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure[J]. Circulation, 2015, 131(1): 54-61.
doi: 10.1161/CIRCULATIONAHA.114.013748 pmid: 25403646 |
| [25] |
LEVIN E R, GARDNER D G, SAMSON W K. Natriuretic peptides[J]. N Engl J Med, 1998, 339(5): 321-328.
doi: 10.1056/NEJM199807303390507 |
| [26] |
MOERTL D, BERGER R, STRUCK J, et al. Comparison of midregional pro-atrial and B-type natriuretic peptides in chronic heart failure: influencing factors, detection of left ventricular systolic dysfunction, and prediction of death[J]. J Am Coll Cardiol, 2009, 53(19): 1783-1790.
doi: 10.1016/j.jacc.2009.01.057 pmid: 19422985 |
| [27] |
PONIKOWSKI P, VOORS A A, ANKER S D, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. The task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC[J]. Eur Heart J, 2016, 37(27): 2129-2200.
doi: 10.1093/eurheartj/ehw128 |
| [28] |
ZHANG Y S, KNIGHT W, CHEN S, et al. Multiprotein complex with TRPC (transient receptor potential-canonical) channel, PDE1C (phosphodiesterase 1C), and A2R (adenosine A2 receptor) plays a critical role in regulating cardiomyocyte cAMP and survival[J]. Circulation, 2018, 138(18): 1988-2002.
doi: 10.1161/CIRCULATIONAHA.118.034189 pmid: 29871977 |
| [29] |
INSEL J, MIRVIS D M, BOLAND M J, et al. A multicenter study of the safety and efficacy of benazepril hydrochloride, a long-acting angiotensin-converting enzyme inhibitor, in patients with chronic congestive heart failure[J]. Clin Pharmacol Ther, 1989, 45(3): 312-320.
pmid: 2537699 |
| [30] |
COLLABORATION A R B T. Effects of telmisartan, irbesartan, valsartan, candesartan, and losartan on cancers in 15 trials enrolling 138 769 individuals[J]. J Hypertens, 2011, 29(4): 623-635.
doi: 10.1097/HJH.0b013e328344a7de |
| [31] |
HO C Y, DAY S M, AXELSSON A, et al. Valsartan in early-stage hypertrophic cardiomyopathy: a randomized phase 2 trial[J]. Nat Med, 2021, 27(10): 1818-1824.
doi: 10.1038/s41591-021-01505-4 pmid: 34556856 |
| [32] |
RURIK J G, TOMBÁCZ I, YADEGARI A, et al. CAR T cells produced in vivo to treat cardiac injury[J]. Science, 2022, 375(6576): 91-96.
doi: 10.1126/science.abm0594 |
| [33] |
DESAI A S, MCMURRAY J J, PACKER M, et al. Effect of the angiotensin-receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patients[J]. Eur Heart J, 2015, 36(30): 1990-1997.
doi: 10.1093/eurheartj/ehv186 pmid: 26022006 |
| [34] |
GE Q, ZHAO L, REN X M, et al. LCZ696, an angiotensin receptor-neprilysin inhibitor, ameliorates diabetic cardiomyopathy by inhibiting inflammation, oxidative stress and apoptosis[J]. Exp Biol Med (Maywood), 2019, 244(12): 1028-1039.
doi: 10.1177/1535370219861283 pmid: 31262190 |
| [35] |
MIZUTA Y, TOKUDA K, GUO J, et al. Sodium thiosulfate prevents doxorubicin-induced DNA damage and apoptosis in cardiomyocytes in mice[J]. Life Sci, 2020, 257: 118074.
doi: 10.1016/j.lfs.2020.118074 |
| [36] | CHILDS A C, PHANEUF S L, DIRKS A J, et al. Doxorubicin treatment in vivo causes cytochrome C release and cardiomyocyte apoptosis, as well as increased mitochondrial efficiency, superoxide dismutase activity, and Bcl-2: Bax ratio[J]. Cancer Res, 2002, 62(16): 4592-4598. |
| [37] |
MALEK V, GAIKWAD A B. Telmisartan and thiorphan combination treatment attenuates fibrosis and apoptosis in preventing diabetic cardiomyopathy[J]. Cardiovasc Res, 2018, 115(2): 373-384.
doi: 10.1093/cvr/cvy226 |
| [38] |
SABBAH H N. Silent disease progression in clinically stable heart failure[J]. Eur J Heart Fail, 2017, 19(4): 469-478.
doi: 10.1002/ejhf.705 pmid: 27976514 |
| [39] |
JIA W K, BAI T, ZENG J, et al. Combined administration of metformin and atorvastatin attenuates diabetic cardiomyopathy by inhibiting inflammation, apoptosis, and oxidative stress in type 2 diabetic mice[J]. Front Cell Dev Biol, 2021, 9: 634900.
doi: 10.3389/fcell.2021.634900 |
| [40] |
WANG Z Q, CHEN M T, ZHANG R, et al. Docosahexaenoic acid attenuates doxorubicin-induced cytotoxicity and inflammation by suppressing NF-κB/iNOS/NO signaling pathway activation in H9C2 cardiac cells[J]. J Cardiovasc Pharmacol, 2016, 67(4): 283-289.
doi: 10.1097/FJC.0000000000000350 |
| [41] | WANG Y B, LIU L. Effects of carvedilol on myocardial remodeling, oxidative stress, inflammation indexes and endothelial function in hypertensive rats[J]. Minerva Surg, 2021. |
| [42] | ALANAZI A M, FADDA L, ALHUSAINI A, et al. Liposomal resveratrol and/or carvedilol attenuate doxorubicin-induced cardiotoxicity by modulating inflammation, oxidative stress and S100A1 in rats[J]. Antioxidants (Basel), 2020, 9(2): E159. |
| [43] |
BANGALORE S, KUMAR S, KJELDSEN S E, et al. Antihypertensive drugs and risk of cancer: network meta-analyses and trial sequential analyses of 324 168 participants from randomised trials[J]. Lancet Oncol, 2011, 12(1): 65-82.
doi: 10.1016/S1470-2045(10)70260-6 |
| [44] |
KEATING G M, JARVIS B. Carvedilol: a review of its use in chronic heart failure[J]. Drugs, 2003, 63(16): 1697-1741.
pmid: 12904089 |
| [45] |
SIPAHI I, DEBANNE S M, ROWLAND D Y, et al. Angiotensin-receptor blockade and risk of cancer: meta-analysis of randomised controlled trials[J]. Lancet Oncol, 2010, 11(7): 627-636.
doi: 10.1016/S1470-2045(10)70106-6 pmid: 20542468 |
| [1] | WU Zhibai, XU Guiqin, ZHANG Li, YANG Zhaojuan, LIU Yun, JIAO Kun, CHEN Zehong, XU Chen, ZUO You, ZHENG Ningqian, YE Zhiqian, LIU Yongzhong. Mechanism study of KCMF1 promoting proliferation and NF-κB signaling transduction in colorectal cancer cells [J]. China Oncology, 2024, 34(11): 987-997. |
| [2] | CHEN Hong, CHEN Junxia. Effect of hsa_circ_0001573 on biological behaviors of breast cancer cells and its molecular mechanism [J]. China Oncology, 2023, 33(4): 342-353. |
| [3] | Diao Xinfeng, Li Xinmao, Hou Liang, Wei Zhixuan. YTHDF2 promotes progression of glioblastoma via inducing mRNA decay of IGFBP7 and activating PI3K/AKT signaling pathway [J]. China Oncology, 2022, 32(3): 218-227. |
| [4] | CAO Dalong, YE Dingwei. New trends and future prospects of regulatory cell death in renal carcinoma [J]. China Oncology, 2022, 32(10): 1000-1006. |
| [5] | LI Mengjuan, LIU Ying, ZHANG Yanli, LIU Mengyao, XUE Yanan, SU Liping, ZHANG Xiujie, SHI Tieying, FANG Fengqi, LIU Jiwei, XIA Yunlong. Current status and research hotspots of cardio-oncology based on bibliometrics [J]. China Oncology, 2022, 32(10): 925-935. |
| [6] | ZHANG Qingling, ZHANG Yunpeng, ZHOU Zandong, ZHANG Yue, LIU Tong. Construction of a mouse model of adriamycin-induced cardiomyopathy [J]. China Oncology, 2022, 32(10): 948-959. |
| [7] | XU Xiaofei, ZHANG Lixia, DAI Heyang, CHEN Lingyun, XUE Jiaojiao, LI Qingxia. Value of global longitudinal strain in assessing radiation-induced heart disease in breast cancer: systematic review and meta-analysis [J]. China Oncology, 2022, 32(10): 971-978. |
| [8] | MA Yifei , LIANG Xinjun , WEI Shaozhong . Prognostic value of inflammatory and immune markers in resectable colorectal cancer [J]. China Oncology, 2021, 31(9): 845-851. |
| [9] | LI Haizhou , ZHANG Yanwei , XU Yingjie , YANG Men , ZHANG Lei , HAN Jingjun . miR-933 inhibits proliferation, migration and invasion of lung cancer cell lines by regulation of KLF6 gene [J]. China Oncology, 2021, 31(7): 581-588. |
| [10] | CAO Dalong, ZHU Wenkai, SHI Guohai, ZHANG Hailiang, WANG Ziliang, YE Dingwei. The influence of PRUNE2 gene point mutation on proliferation, apoptosis, invasion and migration of prostate cancer DU145 cells [J]. China Oncology, 2021, 31(6): 441-446. |
| [11] | HUA Qing, SHEN Xuefang, XU Pingbo . Effect of KLK8 on apoptosis of colorectal cancer cells by regulating EGF and its mechanism [J]. China Oncology, 2021, 31(5): 383-389. |
| [12] | CHEN Guo , HAN Pengli , CHEN Keru , LI Mingchuang , ZHANG Qingsong , CHEN Zheng , DONG Hanhua , QIAN Yuejun , LÜ Jing . Molecular mechanism of miR-19b-3p regulating apoptosis of medullary thyroid cancer cells by targeting MTUS1 [J]. China Oncology, 2021, 31(5): 390-396. |
| [13] | CHEN Shaogeng, HE Rongqi, ZHANG Wanfei, LIN Xianzuan, CHEN Heshan, XU Rongyu. miR-122-5p inhibits the growth of esophageal cancer cells and transplanted tumors by targeting CREB1 [J]. China Oncology, 2021, 31(1): 35-44. |
| [14] | OUYANG Xiaochun , ZOU Yeqing , LI Yumei , DING Xiaobing . ARHGAP4 promotes growth of hepatocellular carcinoma cells by regulating HK2 expression [J]. China Oncology, 2020, 30(7): 481-487. |
| [15] | WANG Fang , WANG Xin , LIU Zhe , HUI Lingyun , FENG Ai , LI Na , WANG Yawen . Inhibition of PDK1 induces apoptosis in CML cells via activation of ASK1/JNK/Bim cascade [J]. China Oncology, 2020, 30(6): 401-406. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
