Welcome to China Oncology,
China Oncology ›› 2022, Vol. 32 ›› Issue (2): 161-171.doi: 10.19401/j.cnki.1007-3639.2022.02.008
Previous Articles Next Articles
Received:2021-05-30
Revised:2022-01-05
Online:2022-02-28
Published:2022-03-08
Contact:
JIN Zhengming
E-mail:jinzhengming519519@163.com
Share article
CLC Number:
JIN Zhengming. Clinical practice optimization exploration and future prospects of autologous hematopoietic stem cell transplantation for lymphoma[J]. China Oncology, 2022, 32(2): 161-171.
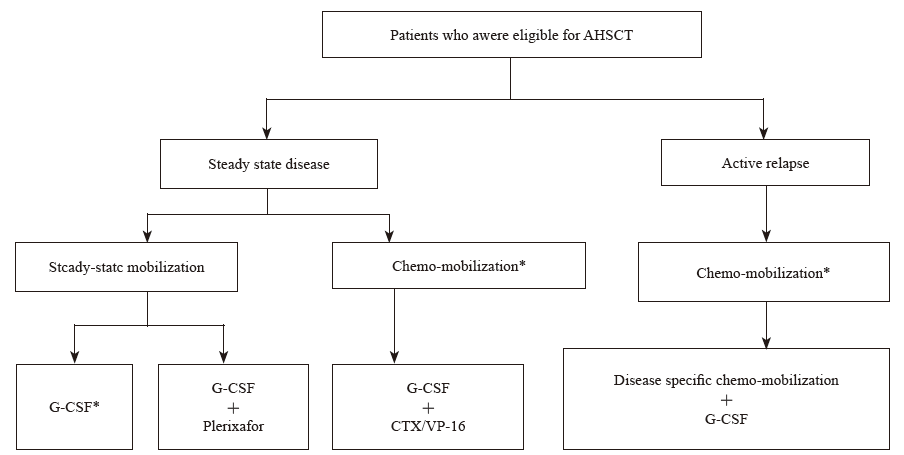
Fig. 2
Mobilization algorithm of PBSC *: For PBSC mobilization with G-CSF alone or in combination with chemotherapy, the introduction of plerixafor are recommended as rescue treatment in the following situations: ① PB CD34+ cell count prior to apheresis<10/µL, pre-emptive plerixafor; ② pre-apheresis PB CD34+ cell count between10-20/µL, consider whether to use plerixafor based on the impact of poor mobilization, planned number of transplants and total amount of stem cells required (if day 1 yield<1.5×106 CD34+/kg add plerixafor; if yield beyond day 1<0.5×106 CD34+/kg add plerixafor)."
Tab. 1
Management of adverse events following AHSCT"
| Adverse events | Management strategies |
|---|---|
| Nausea/vomiting | Antiemetics |
| Diarrhea | Antidiarrheals and fluids to prevent dehydration |
| Loss of appetite | Dexamethasone to stimulate appetite |
| Altered taste sensation | Zinc tablets or lemon candy |
| Mucositis | Pelifermin, anesthetic mouth wash, supersaturated calcium phosphate |
| oral rinse, opioid analgesic, parenteral nutrition in severe case | |
| Myelosuppression | G-CSF, blood component transfusions |
| Fevers | Evaluate for infections, antipyretics |
| Fatigue | Exercise |
| Infections (bacterial, viral, fungal, etc.) | Symptomatic and supportive care as appropriate based on etiological analysis with reference to international guidelines. For patients with pneumocystis jiroveci pneumonia, recommend dapsone 50 mg and atovaquone 750 mg orally daily as 2 divided doses |
| Clostridium difficile diarrhea | Hand washing/metronidazole, oral vancomycin |
| Hemorrhagic cystitis | Mesna for prophylaxi |
| Cataracts | Topical corticosteroids or emollients |
| Parotitis | Chewing gums, lemon drops |
| Infertility | Sperm or oocyte cryopreservation |
| Hypothyroidism/osteoporosis | Avoid TBI |
| Flushing/hypotension/breath odor due to DMSO/allergic reactions/ chest tightness/dyspnea | Slow down infusion rate or give acetaminophen, histamine blockers, corticosteroids |
| Atrial fibrillation | Beta-blockers and calcium channel blockers should be used for rhythm management; anticoagulation therapy to prevent stroke and potential risk factors management |
| [1] | JIANG M L,, BENNANI N N,, FELDMAN A L. Lymphoma classification update: T-cell lymphomas, Hodgkin lymphomas, and histiocytic/dendritic cell neoplasms[J]. Expert Rev Hematol, 2017,10(3):239-249. |
| [2] | SHANKLAND K R,, ARMITAGE J O,, HANCOCK B W. Non-Hodgkin lymphoma[J]. Lancet, 2012,380(9844):848-857. |
| [3] | 石远凯,, 孙燕. 中国恶性实体瘤自体造血干细胞移植25年回顾[J]. 中华医学杂志, 2015,95(10):721-726. |
| SHI Y K,, SUN Y. Review of autologous hematopoietic stem cell transplantation for malignant solid tumors in China for 25 years[J]. Natl Med J China, 2015,95(10):721-726. | |
| [4] | COLITA A,, COLITA A,, BUMBEA H, et al. LEAM vs BEAM vs CLV conditioning regimen for autologous stem cell transplantation in malignant lymphomas. Retrospective comparison of toxicity and efficacy on 222 patients in the first 100 days after transplant, on behalf of the Romanian Society for Bone Marrow Transplantation[J]. Front Oncol, 2019,9:892. |
| [5] | XU L P,, LU P H,, WU D P, et al. Hematopoietic stem cell transplantation activity in China 2019: a report from the Chinese Blood and Marrow Transplantation Registry Group[J]. Bone Marrow Transplant, 2021,56(12):2940-2947. |
| [6] | 吴冠青,, 雷英衡,, 孙燕, 等. 大剂量放化疗合并自体骨髓移植治疗成人晚期高度恶性T细胞非何杰金淋巴瘤[J]. 中华肿瘤杂志, 1993,15(1):47-51. |
| WU G Q,, LEI Y H,, SUN Y, et al. High dose radiotherapy and chemotherapy combined with autologous bone marrow transplantation in the treatment of adult advanced highly malignant T-cell non-Hodgkin’s lymphoma[J]. Chin J Oncol, 1993,15(1):47-51. | |
| [7] | KANATE A S,, MAJHAIL N S,, SAVANI B N, et al. Indications for hematopoietic cell transplantation and immune effector cell therapy: guidelines from the American Society for Transplantation and Cellular Therapy[J]. Biol Blood Marrow Transplant, 2020,26(7):1247-1256. |
| [8] | NCCN. NCCN Clinical Practice Guidelines in Oncology[M]. B-cell lymphomas, version 5, September 22, 2021. |
| [9] | DUARTE R F,, LABOPIN M,, BADER P, et al. Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019[J]. Bone Marrow Transplant, 2019,54(10):1525-1552. |
| [10] | 中国临床肿瘤学会. 淋巴瘤诊疗指南(2021)[M]. 北京: 人民卫生出版社: 1-292. |
| Chinese Society of Clinical Oncology. Guidelines for diagnosis and treatment of lymphoma (2021) [M]. Beijing, People’s Medical Publishing House: 1-292. | |
| [11] | MILPIED N,, DECONINCK E,, GAILLARD F, et al. Initial treatment of aggressive lymphoma with high-dose chemotherapy and autologous stem-cell support[J]. N Engl J Med, 2004,350(13):1287-1295. |
| [12] | GREB A,, BOHLIUS J,, TRELLE S, et al. High-dose chemotherapy with autologous stem cell support in first-line treatment of aggressive non-Hodgkin lymphoma - results of a comprehensive meta-analysis[J]. Cancer Treat Rev, 2007,33(4):338-346. |
| [13] | STIFF P J,, UNGER J M,, COOK J R, et al. Autologous transplantation as consolidation for aggressive non-Hodgkin’s lymphoma[J]. N Engl J Med, 2013,369(18):1681-1690. |
| [14] | HAMADANI M,, HARI P N,, ZHANG Y, et al. Early failure of frontline rituximab-containing chemo-immunotherapy in diffuse large B cell lymphoma does not predict futility of autologous hematopoietic cell transplantation[J]. Biol Blood Marrow Transplant, 2014,20(11):1729-1736. |
| [15] | VILLA D,, SEHN L H,, SAVAGE K J, et al. Bendamustine and rituximab as induction therapy in both transplant-eligible and-ineligible patients with mantle cell lymphoma[J]. Blood Adv, 2020,4(15):3486-3494. |
| [16] | 中国抗癌协会血液肿瘤专业委员会, 中华医学会血液学分会白血病淋巴瘤学组, 中国临床肿瘤学会抗淋巴瘤联盟. 造血干细胞移植治疗淋巴瘤中国专家共识(2018版)[J]. 中华肿瘤杂志, 2018,40(12):927-934. |
| Hematology Oncology Committee of China Anti-Cancer Association, Leukemia & Lymphoma Group; Society of Hematology at Chinese Medical Association, Chinese Union of Lymphoma Research; Chinese Society of Clinical Oncology. The Chinese expert consensus on hematopoietic stem cell transplantation for malignant lymphoma(2018)[J]. Chin J Oncol, 2018,40(12):927-934. | |
| [17] | YAMASAKI S,, CHIHARA D,, KIM S W, et al. Risk factors and timing of autologous stem cell transplantation for patients with peripheral T-cell lymphoma[J]. Int J Hematol, 2019,109(2):175-186. |
| [18] | HAN X,, ZHANG W,, ZHOU D B, et al. Autologous stem cell transplantation as frontline strategy for peripheral T-cell lymphoma: a single-centre experience[J]. J Int Med Res, 2017,45(1):290-302. |
| [19] | CHESON B D,, FISHER R I,, BARRINGTON S F, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification[J]. J Clin Oncol, 2014,32(27):3059-3068. |
| [20] | DEVINE S M. Toward a more rational policy for autologous hematopoietic stem cell mobilization[J]. Biol Blood Marrow Transplant, 2012,18(10):1468-1470. |
| [21] | MOHTY M,, HÜBEL K,, KRÖGER N, et al. Autologous haematopoietic stem cell mobilisation in multiple myeloma and lymphoma patients: a position statement from the European Group for Blood and Marrow Transplantation[J]. Bone Marrow Transplant, 2014,49(7):865-872. |
| [22] | GIRALT S,, COSTA L,, SCHRIBER J, et al. Optimizing autologous stem cell mobilization strategies to improve patient outcomes: consensus guidelines and recommendations[J]. Biol Blood Marrow Transplant, 2014,20(3):295-308. |
| [23] | FRICKER S P,, ANASTASSOV V,, COX J, et al. Characterization of the molecular pharmacology of AMD3100: a specific antagonist of the G-protein coupled chemokine receptor, CXCR4[J]. Biochem Pharmacol, 2006,72(5):588-596. |
| [24] | LUND T,, GLASS T,, TOLAR J, et al. A model system for visualization of whole-body sdf-1 expression during hematopoietic cell transplant[J]. Blood, 2009,114(22):3623. |
| [25] | DIPERSIO J F,, MICALLEF I N,, STIFF P J, et al. Phase Ⅲ prospective randomized double-blind placebo-controlled trial of plerixafor plus granulocyte colony-stimulating factor compared with placebo plus granulocyte colony-stimulating factor for autologous stem-cell mobilization and transplantation for patients with non-Hodgkin’s lymphoma[J]. J Clin Oncol, 2009,27(28):4767-4773. |
| [26] | ZHU J,, HUANG H Q,, CHEN H, et al. Plerixafor and granulocyte-colony-stimulating factor for mobilization of hematopoietic stem cells for autologous transplantation in Chinese patients with non-Hodgkin’s lymphoma: a randomized Phase 3 study[J]. Transfusion, 2018,58(1):81-87. |
| [27] | SHAUGHNESSY P,, ISLAS-OHLMAYER M,, MURPHY J, et al. Cost and clinical analysis of autologous hematopoietic stem cell mobilization with G-CSF and plerixafor compared to G-CSF and cyclophosphamide[J]. Biol Blood Marrow Transplant, 2011,17(5):729-736. |
| [28] | ADEL N G,, DUCK E,, COLLUM K, et al. Cost analysis of using plerixafor plus G-CSF versus cyclophosphamide plus G-CSF for autologous stem cell mobilization in multiple myeloma patients treated at Memorial Sloan-Kettering Cancer Center (MSKCC)[J]. Blood, 2011,118(21):4059. |
| [29] | CAMPEN C J,, ARMSTRONG E P,, CHRISTIAN J A, et al. Comparative cost-effectiveness of plerixafor plus granulocyte-colony stimulating factor versus cyclophosphamide plus granulocyte-colony stimulating for autologous peripheral blood stem cell mobilization in patients with non-Hodgkin’s lymphoma[J]. Biol Blood Marrow Transplant, 2010,16(2):S206. |
| [30] | DANYLESKO I,, SARELI R,, VARDA-BLOOM N, et al. Plerixafor (mozobil): a stem cell-mobilizing agent for transplantation in lymphoma patients predicted to be poor mobilizers-a pilot study[J]. Acta Haematol, 2016,135(1):29-36. |
| [31] | GERTZ M A. Current status of stem cell mobilization[J]. Br J Haematol, 2010,150(6):647-662. |
| [32] | CARRERAS E,, DUFOUR C,, MOHTY M, et al. The EBMT handbook: hematopoietic stem cell transplantation and cellular therapies[M]. Cham: Springer, 2019. |
| [33] | JANTUNEN E,, VARMAVUO V,, VALTOLA J. Plerixafor injection: a hematopoietic stem cell mobilizer in non-Hodgkin lymphoma and multiple myeloma[J]. Expert Rev Hematol, 2016,9(8):723-732. |
| [34] | HAN X H,, MA L,, ZHAO L D, et al. Predictive factors for inadequate stem cell mobilization in Chinese patients with NHL and HL: 14-year experience of a single-center study[J]. J Clin Apher, 2012,27(2):64-74. |
| [35] | CALANDRA G,, MCCARTY J,, MCGUIRK J, et al. AMD3100 plus G-CSF can successfully mobilize CD34 + cells from non-Hodgkin’s lymphoma, Hodgkin’s disease and multiple myeloma patients previously failing mobilization with chemotherapy and/or cytokine treatment: compassionate use data [J]. Bone Marrow Transplant, 2008,41(4):331-338. |
| [36] | VARMAVUO V,, MÄNTYMAA P,, KUITTINEN T, et al. Pre-emptive plerixafor injection increases blood neutrophil, lymphocyte and monocyte counts in addition to CD34 + counts in patients with non-Hodgkin lymphoma mobilizing poorly with chemotherapy plus G-CSF: potential implications for apheresis and graft composition [J]. Transfus Apher Sci, 2012,46(3):257-262. |
| [37] | SÁNCHEZ-ORTEGA I,, QUEROL S,, ENCUENTRA M, et al. Plerixafor in patients with lymphoma and multiple myeloma: effectiveness in cases with very low circulating CD34 + cell levels and preemptive intervention vs remobilization [J]. Bone Marrow Transplant, 2015,50(1):34-39. |
| [38] | DUONG H K,, SAVANI B N,, COPELAN E, et al. Peripheral blood progenitor cell mobilization for autologous and allogeneic hematopoietic cell transplantation: guidelines from the American Society for Blood and Marrow Transplantation[J]. Biol Blood Marrow Transplant, 2014,20(9):1262-1273. |
| [39] | LEBEL E,, LAJKOSZ K,, MASIH-KHAN E, et al. Supermobilizers with high CD34 + cell collection for autologous transplant and impact on survival outcomes in multiple myeloma [J]. Blood, 2021,138:1837. |
| [40] | PORRATA L F,, BURGSTALER E A,, WINTERS J L, et al. Immunologic autograft engineering and survival in non-Hodgkin lymphoma[J]. Biol Blood Marrow Transplant, 2016,22(6):1017-1023. |
| [41] | FURLONG E,, JENSEN J,, WOODARD M, et al. Optimized peripheral blood progenitor cell mobilization for autologous hematopoietic cell transplantation in children with high-risk and refractory malignancies[J]. Pediatr Transplant, 2020,24(1):e13602. |
| [42] | LECCHI L,, GIOVANELLI S,, GAGLIARDI B, et al. An update on methods for cryopreservation and thawing of hemopoietic stem cells[J]. Transfus Apher Sci, 2016,54(3):324-336. |
| [43] | AKKÖK C A,, LISETH K,, MELVE G K, et al. Is there a scientific basis for a recommended standardization of collection and cryopreservation of peripheral blood stem cell grafts?[J]. Cytotherapy, 2011,13(8):1013-1024. |
| [44] | 俞立权. 造血干细胞移植标准实践手册[M]. 北京: 人民卫生出版社, 2007. |
| YU L Q. Standard practice manual for hematopoietic stem cell transplantation[M]. Beijing: People’s Medical Publishing House Co., LTD, 2007. | |
| [45] | SHI Y W,, LIU P,, ZHOU S Y, et al. Comparison of CBV, BEAM and BEAC high-dose chemotherapy followed by autologous hematopoietic stem cell transplantation in non-Hodgkin lymphoma: efficacy and toxicity[J]. Asia Pac J Clin Oncol, 2017,13(5):e423-e429. |
| [46] | VELA-OJEDA J,, GARCÍA-RUIZ-ESPARZA M A,, PADILLA-GONZÁLEZ Y, et al. Autologous peripheral blood stem cell transplantation in multiple myeloma using oral versus I.V. melphalan[J]. Ann Hematol, 2007,86(4):277-282. |
| [47] | HUANG H W,, ZHANG L H,, JIANG Y B, et al. Modified BuCy is an alternative conditioning regimen for lymphoma patients undergoing autologous stem cell transplantation[J]. Ann Hematol, 2019,98(5):1259-1266. |
| [48] | 何旭,, 季杰,, 马春蓉, 等. 氟达拉滨联合BEAM预处理自体外周血干细胞移植治疗非霍奇金淋巴瘤的效果[J]. 国际移植与血液净化杂志, 2017,15(5):24-27. |
| HE X,, JI J,, MA C R, et al. Effect of fludarabine combined with beam pretreatment autologous peripheral blood stem cell transplantation in the treatment of non-Hodgkin’s lymphoma[J]. Int J Transplant Blood Purification, 2017,15(5):24-27. | |
| [49] | ELEMARY M,, SEGHATCHIAN J,, STAKIW J, et al. Transfusion challenges in hematology oncology and hematopoietic stem cell transplant - literature review and local experience[J]. Transfus Apher Sci, 2017,56(3):317-321. |
| [50] | TOMBLYN M,, CHILLER T,, EINSELE H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective[J]. Bone Marrow Transplant, 2009,44(8):453-455. |
| [51] | HAMADANI M. Autologous hematopoietic cell transplantation: an update for clinicians[J]. Ann Med, 2014,46(8):619-632. |
| [52] | HIJAZI Z,, OLDGREN J,, ANDERSSON U, et al. Cardiac biomarkers are associated with an increased risk of stroke and death in patients with atrial fibrillation: a randomized evaluation of long-term anticoagulation therapy (RE-LY) substudy[J]. Circulation, 2012,125(13):1605-1616. |
| [53] | KANATE A S,, KUMAR A,, DREGER P, et al. Maintenance therapies for Hodgkin and non-Hodgkin lymphomas after autologous transplantation: a consensus project of ASBMT, CIBMTR, and the lymphoma working party of EBMT[J]. JAMA Oncol, 2019,5(5):715-722. |
| [54] | MADDOCKS K,, BLUM K A. Treatment strategies in mantle cell lymphoma[J]. Cancer Treat Res, 2015,165:251-270. |
| [55] | MAJHAIL N S,, RIZZO J D,, LEE S J, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation[J]. Biol Blood Marrow Transplant, 2012,18(3):348-371. |
| [1] | Cancer Nuclear Medicine Committee of China Anti-Cancer Association, Chinese Association of Nuclear Medicine Physicians. Expert consensus of 177Lu-labeled PSMA radioligand therapy for clinical practice of prostate cancer (2024 edition) [J]. China Oncology, 2024, 34(7): 702-714. |
| [2] | LIN Jiaxin, WEI Ran, SHUI Ruohong, LU Hongfen, LI Xiaoqiu, YU Baohua. Clinicopathological analysis of adrenal intravascular large B-cell lymphoma [J]. China Oncology, 2024, 34(11): 1020-1027. |
| [3] | WEI Jing, HE Yaqi, XUE Tian, BAI Qianming, SHUI Ruohong, LU Hongfen, LI Xiaoqiu, YU Baohua. Clinicopathological analysis of DLBCL/HGBL with MYC, BCL2 and BCL6 gene rearrangement [J]. China Oncology, 2023, 33(9): 809-817. |
| [4] | CD-Positive Lymphoma Pathology Expert Group. The standardization of immunohistochemical detection and interpretation of CD30 expression in lymphomas [J]. China Oncology, 2023, 33(3): 228-234. |
| [5] | HE Liyuan, WANG Yudong. Research progress of ALK kinase domain drug resistance mutation and its future countermeasures [J]. China Oncology, 2022, 32(8): 736-746. |
| [6] | LIU Yanquan, HU Xiaomei, YIN Yue, LIN Lin, SHEN Jianzhen, CHEN Yuting, TANG Huanwen. A retrospective study and clinical analysis of post-transplant lymphoproliferative disorder [J]. China Oncology, 2022, 32(7): 650-656. |
| [7] | LI Xiaoqiu, CD30 Positive Lymphoma Pathology Expert Group. Detection of CD30 expression in lymphomas: status and challenges [J]. China Oncology, 2022, 32(6): 512-518. |
| [8] | CHEN Guangliang, WU Fangtian, CAO Junning. Advances in research on EBV positive diffuse large B-cell lymphoma, not otherwise specified [J]. China Oncology, 2022, 32(3): 258-267. |
| [9] | Tumor Support and Rehabilitation Therapy Group, the Oncology Committee of Chinese Medical Association. Clinical practice guidelines for cancer-related fatigue in China (2021 edition) [J]. China Oncology, 2021, 31(9): 852-872. |
| [10] | HE Hesheng , YANG Yuqiong , LIU Yinhua , JIN Xiaoke , XU Youhai , YAO Junping , LIU Shanhao , YAN Jiawei , HUANG Dongping . Characteristic analysis of peripheral T-cell lymphoma associated with autoimmune hemolytic anemia [J]. China Oncology, 2021, 31(2): 121-125. |
| [11] | LI Lei , WANG Zhi , YOU Chunyuan . The relapse of primary cardiac high-grade B-cell lymphoma after remission: a case report [J]. China Oncology, 2021, 31(2): 156-160. |
| [12] | LI Panpan, ZHANG Zhuo. Analysis of prognostic factors in 42 cases of primary central nervous system lymphoma [J]. China Oncology, 2021, 31(12): 1194-1201. |
| [13] | QIN Lingyan , GUO Lingchuan , GU Dongmei , YU Jie , YOU Zhiqun , HE Lu . Cytopathological characteristics of pleural effusion in diagnosis of mediastinal diffuse large B-cell lymphoma [J]. China Oncology, 2020, 30(9): 712-717. |
| [14] | ZHANG Yan, TANG Yong, YAO Yiyun, ZOU Lifang, DOU Hongju, ZHU Qi. Retrospective analytical study on clinical features and prognostic models in patients with head and neck diffuse large B-cell lymphoma [J]. China Oncology, 2020, 30(6): 449-455. |
| [15] | GE Xiaowen, YAO Jiamei, ZHU Na, LUAN Lijuan, GAO Feng, ZENG Haiying, JI Yuan, TAN Yunshan, HOU Yingyong. Expression and clinical implication of calreticulin in diffuse large B-cell lymphoma [J]. China Oncology, 2020, 30(5): 347-354. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd

