Welcome to China Oncology,
China Oncology ›› 2025, Vol. 35 ›› Issue (3): 298-308.doi: 10.19401/j.cnki.1007-3639.2025.03.006
• Article • Previous Articles Next Articles
WANG Haochen( ), JIA Liqing, YANG Yu, WANG Qian, YU Chengli, TIAN Tian, BI Rui, TU Xiaoyu, BAI Qianming, ZHU Xiaoli, ZHOU Xiaoyan, REN Min(
), JIA Liqing, YANG Yu, WANG Qian, YU Chengli, TIAN Tian, BI Rui, TU Xiaoyu, BAI Qianming, ZHU Xiaoli, ZHOU Xiaoyan, REN Min( )
)
Received:2024-11-13
Revised:2025-02-06
Online:2025-03-30
Published:2025-04-10
Contact:
REN Min
Supported by:Share article
CLC Number:
WANG Haochen, JIA Liqing, YANG Yu, WANG Qian, YU Chengli, TIAN Tian, BI Rui, TU Xiaoyu, BAI Qianming, ZHU Xiaoli, ZHOU Xiaoyan, REN Min. A study on the correlation between HPV DNA and IHC P16 expression in cervical lesions[J]. China Oncology, 2025, 35(3): 298-308.
Tab. 1
Clinicopathological features of 618 patients with cervical lesions [n (%)]"
| Variable | Case |
|---|---|
| Age at diagnosis/year | |
| ≤40 | 321 (51.9) |
| >40 | 297 (48.1) |
| Pathological type | |
| Squamous cell carcinom | 92 (14.9) |
| Cervical adenocarcinoma | 257 (42.6) |
| Usual-type | 146 (23.6) |
| Mucinous adenocarcinoma | 19 (3.1) |
| Gastric-type | 38 (6.1) |
| Other | 54 (8.7) |
| HSIL | 79 (12.8) |
| LSIL | 105 (17.0) |
| Inflammation | 85 (14.8) |
| Tumor size cm | |
| ≤4 | 171 (27.7) |
| >4 | 156 (25.2) |
| Unknow | 22 (3.6) |
| NA | 269 (43.5) |
| Lymph node metastasis | |
| Yes | 220 (35.6) |
| No | 121 (19.6) |
| Unkonw | 8 (1.3) |
| NA | 269 (43.5) |
| FIGO installment | |
| Ⅰ | 42 (6.8) |
| Ⅱ | 89 (14.4) |
| Ⅲ | 103 (16.7) |
| Ⅳ | 92 (14.9) |
| Unknown | 23 (3.7) |
| NA | 269 (43.5) |
| Treatment | |
| Preoperative treatment | 19 (3.1) |
| Operative treatment | 118 (19.1) |
| Operative+chemoradiotherapy | 205 (33.2) |
| Disease follow-up visits | 248 (40.1) |
| Unknown | 28 (4.5) |
Tab. 2
HPV subtypes features of 618 patients with cervical lesions [n (%)]"
| HPV subtypes | Cervical squamous cell carcinoma | Cervical adenocarcinoma | HSIL | LSIL | Inflammation |
|---|---|---|---|---|---|
| HR-HPV | |||||
| 16 | 55 (59.7) | 68 (26.5) | 18 (22.8) | 17 (16.2) | 7 (8.2) |
| 18 | 10 (10.9) | 62 (24.1) | 7 (8.9) | 8 (7.6) | 4 (4.7) |
| 31 | 8 (8.7) | 2 (0.8) | 8 (10.1) | 2 (1.9) | 1 (1.2) |
| 33 | 2 (2.2) | 2 (0.8) | 8 (10.1) | 7 (6.7) | 0 (0.0) |
| 35 | 0 (0.0) | 0 (0.0) | 1 (1.3) | 1 (1.0) | 0 (0.0) |
| 39 | 0 (0.0) | 1 (0.4) | 1 (1.3) | 1 (1.0) | 0 (0.0) |
| 45 | 1 (1.1) | 6 (2.3) | 3 (3.8) | 0 (0.0) | 0 (0.0) |
| 51 | 0 (0.0) | 0 (0.0) | 2 (2.5) | 12 (11.4) | 0 (0.0) |
| 52 | 3 (3.3) | 1 (0.4) | 6 (7.6) | 17 (16.2) | 3 (3.5) |
| 53 | 2 (2.2) | 0 (0.0) | 1 (1.3) | 5 (4.8) | 3 (3.5) |
| 56 | 1 (1.1) | 0 (0.0) | 0 (0.0) | 4 (3.8) | 0 (0.0) |
| 58 | 2 (2.2) | 0 (0.0) | 6 (8.9) | 10 (9.5) | 0 (0.0) |
| 59 | 3 (3.3) | 0 (0.0) | 2 (2.5) | 3 (2.9) | 0 (0.0) |
| 66 | 1 (1.1) | 1 (0.4) | 0 (0.0) | 5 (4.8) | 2 (2.4) |
| 68 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.9) | 3 (3.5) |
| 83 | 0 (0.0) | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 82 | 0 (0.0) | 0 (0.0) | 2 (2.5) | 1 (1.0) | 0 (0.0) |
| LR-HPV | |||||
| 6 | 0 (0.0) | 0 (0.0) | 3 (3.8) | 2 (1.9) | 1 (1.2) |
| 11 | 0 (0.0) | 1 (0.4) | 1 (1.3) | 5 (4.8) | 0 (0.0) |
| 42 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (3.8) | 0 (0.0) |
| 43 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.9) | 0 (0.0) |
| 81 | 1 (1.1) | 1 (0.4) | 2 (2.5) | 5 (4.8) | 0 (0.0) |
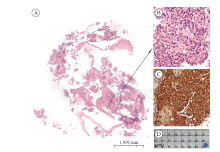
Fig. 2
The case of cervical squamous cell carcinoma with P16 positive and HPV negative A: Low-power scan of the cervical squamous cell carcinoma with about 15% of tumor cell content (the tumor area was highlighted by the circles) (H-E staining, ×10); B: The histological morphology of the cervical squamous cell carcinoma (H-E staining, ×40); C: P16 immunostaining showed positive staining in the tumors; D: Representative PCR showed negative in detection of HPV."
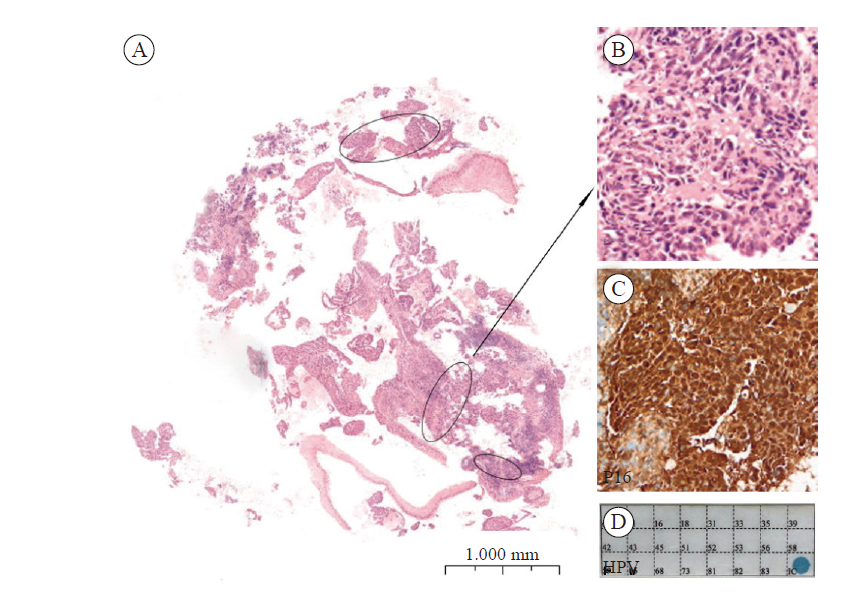
Fig. 3
The case of gastric type cervical adenocarcinoma discrepant findings between IHC-P16 and HPV A: Gastric type cervical adenocarcinoma, non-HPV associated adenocarcinoma (H-E staining, ×20); B: P16 immunostaining showed negitive staining in the tumors; C: A representative PCR positive for HR-HPV DNA; D: Gastric type cervical adenocarcinoma, non-HPV associated adenocarcinoma (H-E staining, ×20); E: P16 immunostaining showed positive staining in the tumors; F: A representative PCR negitive for HR-HPV DNA."
| [1] | MIKAMI Y. Gastric-type mucinous carcinoma of the cervix and its precursors-historical overview[J]. Histopathology, 2020, 76(1): 102-111. |
| [2] | MA X M, HARRIPERSAUD K, SMITH K, et al. Modeling the epidemiological impact and cost-effectiveness of a combined schoolgirl HPV vaccination and cervical cancer screening program among Chinese women[J]. Hum Vaccin Immunother, 2021, 17(4): 1073-1082. |
| [3] | LARQUE A B, CONDE L, HAKIM S, et al. P16 (INK4a) overexpression is associated with CDKN2A mutation and worse prognosis in HPV-negative laryngeal squamous cell carcinomas[J]. Virchows Arch, 2015, 466(4): 375-382. |
| [4] | WANG J L, ZHENG B Y, LI X D, et al. Predictive significance of the alterations of p16INK4A, p14ARF, p53, and proliferating cell nuclear antigen expression in the progression of cervical cancer[J]. Clin Cancer Res, 2004, 10(7): 2407-2414. |
| [5] |
FERRIS R L, WESTRA W. Oropharyngeal carcinoma with a special focus on HPV-related squamous cell carcinoma[J]. Annu Rev Pathol, 2023, 18: 515-535.
doi: 10.1146/annurev-pathmechdis-031521-041424 pmid: 36693202 |
| [6] | KIAN ANG K, HARRIS J, WHEELER R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer[J]. N Engl J Med, 2010, 363(1): 24-35. |
| [7] | DA MATA S, FERREIRA J, NICOLÁS I, et al. P16 and HPV genotype significance in HPV-associated cervical cancer-a large cohort of two tertiary referral centers[J]. Int J Mol Sci, 2021, 22(5): 2294. |
| [8] | RYU A, HONMA K, SHINGETSU A, et al. Utility of p16/Ki-67 double immunocytochemistry for detection of cervical adenocarcinoma[J]. Cancer Cytopathol, 2022, 130(12): 983-992. |
| [9] | ANGELICO G, SANTORO A, INZANI F, et al. An emerging anti-p16 antibody-BC42 clone as an alternative to the current E6H4 for use in the female genital tract pathological diagnosis: our experience and a review on p16ink4a functional significance, role in daily-practice diagnosis, prognostic potential, and technical pitfalls[J]. Diagnostics (Basel), 2021, 11(4): 713. |
| [10] | ZITO MARINO F, SABETTA R, PAGLIUCA F, et al. Discrepancy of p16 immunohistochemical expression and HPV RNA in penile cancer. A multiplex in situ hybridization/immunohistochemistry approach study[J]. Infect Agent Cancer, 2021, 16(1): 22. |
| [11] | BALOCH Z, YASMEEN N, LI Y Y, et al. Knowledge and awareness of cervical cancer, human papillomavirus (HPV), and HPV vaccine among HPV-infected Chinese women[J]. Med Sci Monit, 2017, 23: 4269-4277. |
| [12] |
HE Z M, CHEN R S, HU S Y, et al. The value of HPV genotypes combined with clinical indicators in the classification of cervical squamous cell carcinoma and adenocarcinoma[J]. BMC Cancer, 2022, 22(1): 776.
doi: 10.1186/s12885-022-09826-4 pmid: 35840910 |
| [13] | NAN Z D, DOU Y, CHEN A W, et al. Identification and validation of a prognostic signature of autophagy, apoptosis and pyroptosis-related genes for head and neck squamous cell carcinoma: to imply therapeutic choices of HPV negative patients[J]. Front Immunol, 2023, 13: 1100417. |
| [14] | GIANNELLA L, DI GIUSEPPE J, DELLI CARPINI G, et al. HPV-negative adenocarcinomas of the uterine cervix: from molecular characterization to clinical implications[J]. Int J Mol Sci, 2022, 23(23): 15022. |
| [15] | FUSCONI M, CAMPO F, GALLO A, et al. Laryngeal cancer, HPV DNA vs E6/E7 mRNA test: a systematic review[J]. J Voice, 2017, 31(2): 248.e1-248248.e5. |
| [16] |
GRAVITT P E, PEYTON C L, APPLE R J, et al. Genotyping of 27 human papillomavirus types by using L1 consensus PCR products by a single-hybridization, reverse line blot detection method[J]. J Clin Microbiol, 1998, 36(10): 3020-3027.
doi: 10.1128/JCM.36.10.3020-3027.1998 pmid: 9738060 |
| [17] |
HERNANDEZ J, ELAHI A, SIEGEL E, et al. HPV L1 capsid protein detection and progression of anal squamous neoplasia[J]. Am J Clin Pathol, 2011, 135(3): 436-441.
doi: 10.1309/AJCPR5VD6NSQRWBN pmid: 21350099 |
| [18] | HÖHN A K, BRAMBS C E, HILLER G G R, et al. 2020 WHO classification of female genital tumors[J]. Geburtshilfe Frauenheilkd, 2021, 81(10): 1145-1153. |
| [19] | LUO R Z, CHEN S L, LI M, et al. HPV E6/E7 mRNA in situ hybridization in endocervical adenocarcinoma: implications for prognosis and diagnosis[J]. Cancer Cell Int, 2021, 21(1): 643. |
| [20] | GONZÁLEZ-YEBRA B, MOJICA-LARREA M, ALONSO R, et al. HPV infection profile in cervical lesions[J]. Gac Med Mex, 2022, 158(4): 222-228. |
| [21] | 刘彬, 吴泽妮, 刘潇阳, 等. 人乳头瘤病毒与子宫颈腺癌病因关系研究[J]. 中华肿瘤杂志, 2016, 38(4): 277-282. |
| LIU B, WU Z N, LIU X Y, et al. Distribution of human papillomavirus (HPV) among HPV positive cervical adenocarcinoma cases detected by laser capture microdissection (LCM)[J]. Chin J Oncol, 2016, 38(4): 277-282. | |
| [22] | GAJANIN R, GAJANIN Ž, VUJKOVIĆ Z, et al. Immunohistochemical expression of P16INK4a in inflammatory, preneoplastic and neoplastic cervical lesions[J]. Med Pregl, 2015, 68(3/4): 85-92. |
| [23] | GOTHWAL M, NALWA A, SINGH P, et al. Role of cervical cancer biomarkers p16 and Ki67 in abnormal cervical cytological smear[J]. J Obstet Gynaecol India, 2021, 71(1): 72-77. |
| [24] |
CLARK J L, LU D, KALIR T, et al. Overdiagnosis of HSIL on cervical biopsy: errors in p16 immunohistochemistry implementation[J]. Hum Pathol, 2016, 55: 51-56.
doi: 10.1016/j.humpath.2016.04.010 pmid: 27134110 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
