Welcome to China Oncology,
China Oncology ›› 2024, Vol. 34 ›› Issue (4): 380-388.doi: 10.19401/j.cnki.1007-3639.2024.04.005
• Article • Previous Articles Next Articles
MA Fenghua1( ), JIANG Anqi2,3(
), JIANG Anqi2,3( ), CHEN Yiqing2, XU Congjian2,3(
), CHEN Yiqing2, XU Congjian2,3( ), KANG Yu2,3(
), KANG Yu2,3( )
)
Received:2023-12-29
Revised:2024-04-03
Online:2024-04-30
Published:2024-05-17
Contact:
XU Congjian, KANG Yu
Share article
CLC Number:
MA Fenghua, JIANG Anqi, CHEN Yiqing, XU Congjian, KANG Yu. Magnetic resonance imaging for distinguishing gastric-type endocervical adenocarcinoma from lobular endocervical glandular hyperplasia[J]. China Oncology, 2024, 34(4): 380-388.
Tab. 1
Comparison of clinical features between (atypical) LEGH and G-EAC"
| Clinicopathologic characteristics | LEGH+aLEGH (n=37) | G-EAC (n=53) | P value |
|---|---|---|---|
| Mean age/year | 41.0±10.5 | 46.0±12.0 | 0.015 |
| Manifestations | |||
| Vaginal discharge | 31 (83.8%) | 21 (39.6%) | <0.001 |
| Vaginal bleeding | 2 (5.4%) | 27 (50.9%) | <0.001 |
| Abdominal pain | 0 | 11 (20.8%) | 0.009 |
Tab. 3
Comparison of MRI features between (atypical) LEGH and G-EAC"
| MRI features | LEGH+aLEGH (n = 37) | G-EAC (n = 53) | P value |
|---|---|---|---|
| Extent of lesions | |||
| Epithelial layer | 37 (100.0%) | 11 (20.8%) | <0.001 |
| Muscular layer | 0 (0.0%) | 42 (79.2%) | |
| Mean diameter a/cm | 3.4 ± 1.1 | 4.7 ± 1.6 | <0.001 |
| Components | |||
| Mixed cystic pattern | 19 (51.4%) | 1 (1.9%) | <0.001 |
| Microcystic pattern | 13 (35.1%) | 0 (0.0%) | |
| Mixed cystic-solid pattern | 5 (13.5%) | 16 (30.2%) | |
| Solid pattern | 0 (0.0%) | 36 (67.9%) | |
| Degree of enhancement | |||
| Mild/moderate | 6 (16.2%) | 22 (41.5%) | 0.011 |
| Significant | 31 (83.8%) | 31 (58.5%) | |
| Disrupted cervical stromal ring | 1 (2.7%) | 46 (86.8%) | <0.001 |
| Endometrium invasion | 8 (21.6%) | 34 (64.2%) | <0.001 |
| Ovarian lesions | 7 (18.9%) | 7 (13.2%) | 0.462 |
| Lymph nodes enlargement | 0 (0.0%) | 9 (17.0%) | 0.022 |
| Hydrohystera | 0 (0.0%) | 11 (20.8%) | 0.009 |
| Bladder invasion | 0 (0.0%) | 5 (9.4%) | 0.146 |
Tab. 4
Logistic regression of MRI features"
| MRI features | β | SE | Wald test | OR (95% CI) | P value |
|---|---|---|---|---|---|
| Maximal diameter | -0.141 | 0.379 | 0.138 | 0.868 (0.413-1.827) | 0.710 |
| Components | 3.913 | 1.294 | 9.140 | 50.064 (3.960-632.895) | 0.003 |
| Degree of enhancement | -0.951 | 1.055 | 0.813 | 0.386 (0.049-3.053) | 0.367 |
| Disrupted cervical stromal ring | 3.693 | 1.330 | 7.706 | 40.180 (2.961-545.167) | 0.006 |
| Endometrium invasion | -0.222 | 1.188 | 0.035 | 0.801 (0.078-8.214) | 0.852 |
| Constant | -2.262 | 1.666 | 1.843 | 0.104 | 0.175 |
Tab. 5
ROC analysis of MRI features"
| MRI features | AUC | SE | Asymptotic Sig. | 95% CI |
|---|---|---|---|---|
| Combination | 0.970 | 0.020 | 0.000 | 0.931-1.008 |
| Maximal diameter | 0.747 | 0.052 | 0.000 | 0.644-0.849 |
| Components | 0.923 | 0.035 | 0.000 | 0.854-0.992 |
| Degree of enhancement | 0.374 | 0.059 | 0.032 | 0.258-0.489 |
| Disrupted cervical stromal ring | 0.920 | 0.032 | 0.000 | 0.858-0.983 |
| Endometrium invasion | 0.713 | 0.056 | 0.000 | 0.604-0.822 |
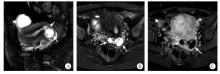
Fig. 2
MRI features of a LEGH patient Sagittal (A) and axial (B) T2WI with fat saturation (FS) showed multiple macrocysts and microcysts with smooth cystic walls in the middle and upper endocervical canal (arrows). Axial contrast-enhanced T1WI with FS (C) showed the cystic walls were significantly enhanced, with no obvious solid component."
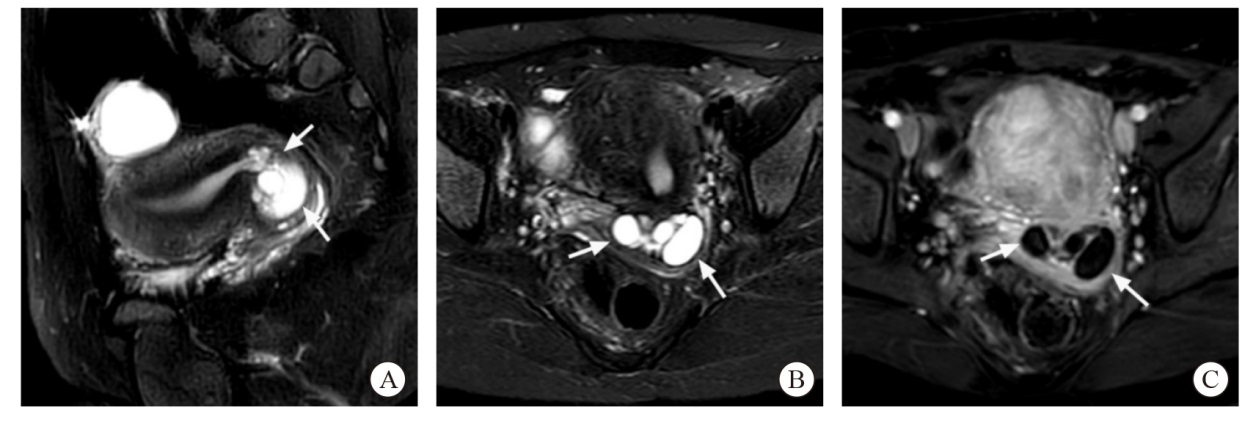

Fig. 3
MRI features of a aLEGH patient Axial (A) and sagittal (B) T2WI with FS showed "cosmos pattern", which was defined as dense microcysts in the center of the lesions surrounded by macrocysts (arrows showed). Sagittal contrast-enhanced T1WI with FS (C) showed dense microcysts with honeycombed enhancement and the walls of macrocysts with mild enhancement."
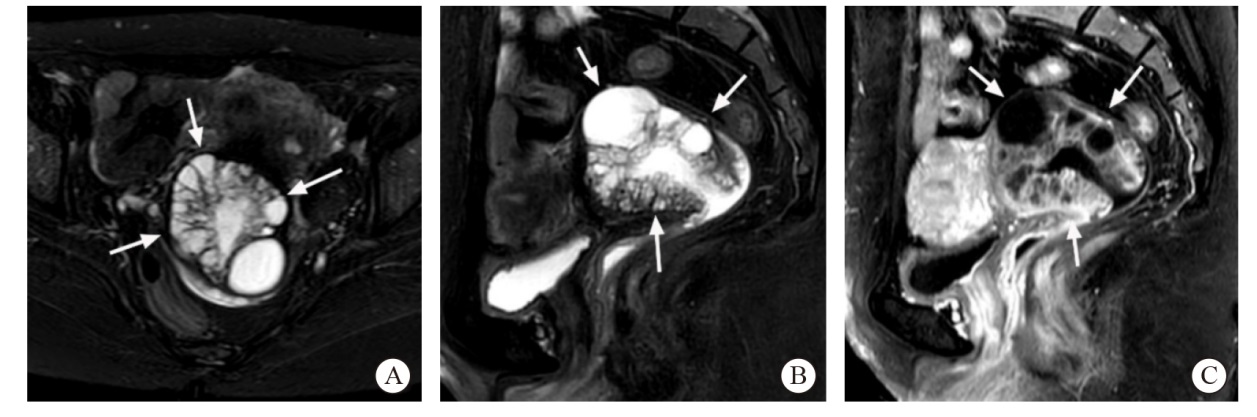

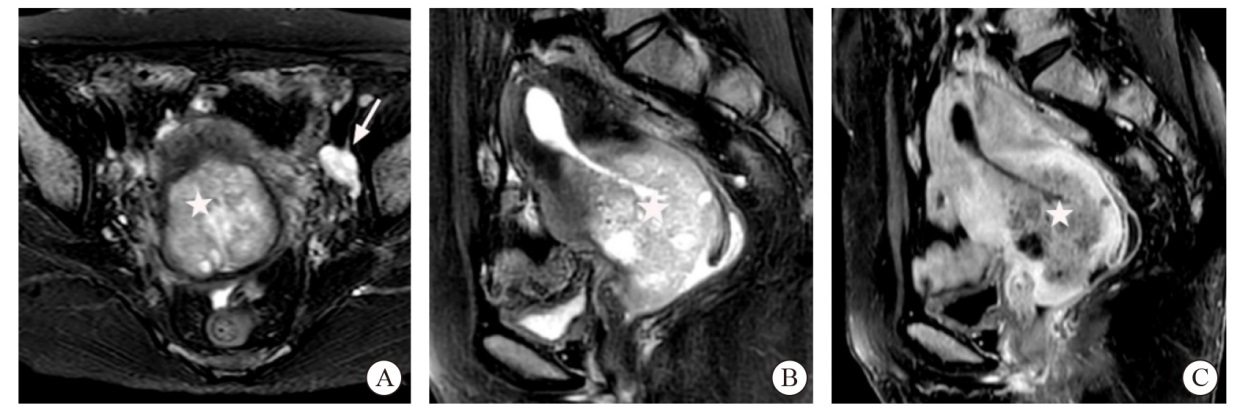
Fig. 4
MRI features of the G-EAC patient case No. 4 Axial (A) and sagittal (B) T2WI with FS showed diffused cystic and solid lesions involving the endometrium and myometrium (arrows) and the cervical stromal ring was missing. Sagittal contrast-enhanced T1WI with FS (C) showed the solid lesions were similar to the enhancement of myometrium and part of cystic walls were significantly enhanced."
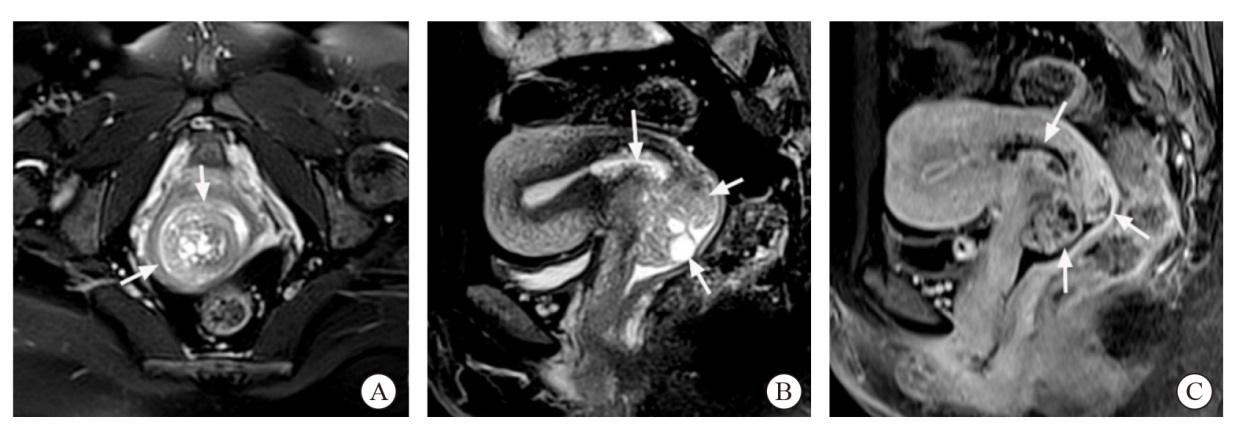

Fig. 5
MRI features of the G-EAC patient case No. 5 Axial (A) and sagittal (B) T2WI with FS showed a solid mass in the endocervical canal (star) involving the endometrium and myometrium and the cervical stromal ring was missing. Enlarged lymph nodes can be seen adjacent to the left iliac vessels (arrow showed). Sagittal contrast-enhanced T1WI with FS (C) showed the solid lesions were mildly enhanced."
| [1] |
NUCCI M R, CLEMENT P B, YOUNG R H. Lobular endocervical glandular hyperplasia, not otherwise specified: a clinicopathologic analysis of thirteen cases of a distinctive pseudoneoplastic lesion and comparison with fourteen cases of adenoma malignum[J]. Am J Surg Pathol, 1999, 23(8): 886-891.
pmid: 10435557 |
| [2] | TALIA K L, MCCLUGGAGE W G. The developing spectrum of gastric-type cervical glandular lesions[J]. Pathology, 2018, 50(2): 122-133. |
| [3] |
EHMANN S, SASSINE D, STRAUBHAR A M, et al. Gastric-type adenocarcinoma of the cervix: clinical outcomes and genomic drivers[J]. Gynecol Oncol, 2022, 167(3): 458-466.
doi: 10.1016/j.ygyno.2022.10.003 pmid: 36253302 |
| [4] |
TAKATSU A, SHIOZAWA T, MIYAMOTO T, et al. Preoperative differential diagnosis of minimal deviation adenocarcinoma and lobular endocervical glandular hyperplasia of the uterine cervix: a multicenter study of clinicopathology and magnetic resonance imaging findings[J]. Int J Gynecol Cancer, 2011, 21(7): 1287-1296.
doi: 10.1097/IGC.0b013e31821f746c pmid: 21685796 |
| [5] |
TSUBOYAMA T, YAMAMOTO K, NAKAI G, et al. A case of gastric-type adenocarcinoma of the uterine cervix associated with lobular endocervical glandular hyperplasia: radiologic-pathologic correlation[J]. Abdom Imaging, 2015, 40(3): 459-465.
doi: 10.1007/s00261-014-0323-6 pmid: 25504516 |
| [6] | YOSHINO A, KOBAYASHI E, TSUBOYAMA T, et al. Novel strategy for the management of cervical multicystic diseases[J]. Ann Surg Oncol, 2023, 30(5): 2964-2973. |
| [7] |
KOBARA H, MIYAMOTO T, ANDO H, et al. Limited frequency of malignant change in lobular endocervical glandular hyperplasia[J]. Int J Gynecol Cancer, 2020, 30(10): 1480-1487.
doi: 10.1136/ijgc-2020-001612 pmid: 32883699 |
| [8] |
NOSÉ V, LAZAR A. Update from the 5th edition of the World Health Organization classification of head and neck tumors: familial tumor syndromes[J]. Head Neck Pathol, 2022, 16: 143-157.
doi: 10.1007/s12105-022-01414-z pmid: 35312981 |
| [9] |
STOLNICU S, BARSAN I, HOANG L, et al. International endocervical adenocarcinoma criteria and classification (IECC): a new pathogenetic classification for invasive adenocarcinomas of the endocervix[J]. Am J Surg Pathol, 2018, 42(2): 214-226.
doi: 10.1097/PAS.0000000000000986 pmid: 29135516 |
| [10] | 吕炳建, 石海燕, 邵颖, 等. 基于国际颈管腺癌标准与分类286例宫颈腺癌临床病理与预后分析[J]. 中华病理学杂志, 2021, 50(9): 1014-1019. |
| LÜ B J, SHI H Y, SHAO Y, et al. Endocervical adenocarcinomas classified by International Endocervical Adenocarcinoma Criteria and Classification: a clinicopathological and prognostic analysis of 286 cases[J]. Chin J Pathol, 2021, 50(9): 1014-1019. | |
| [11] |
SALIB M Y, RUSSELL J H B, STEWART V R, et al. 2018 FIGO staging classification for cervical cancer: added benefits of imaging[J]. Radiographics, 2020, 40(6): 1807-1822.
doi: 10.1148/rg.2020200013 pmid: 32946322 |
| [12] |
XIAO M L, YAN B C, LI Y, et al. Diagnostic performance of MR imaging in evaluating prognostic factors in patients with cervical cancer: a meta-analysis[J]. Eur Radiol, 2020, 30(3): 1405-1418.
doi: 10.1007/s00330-019-06461-9 pmid: 31776741 |
| [13] | SALEH M, VIRARKAR M, JAVADI S, et al. Cervical cancer: 2018 revised international federation of gynecology and obstetrics staging system and the role of imaging[J]. AJR Am J Roentgenol, 2020, 214(5): 1182-1195. |
| [14] | 中国医师协会妇产科医师分会妇科肿瘤学组. 子宫颈胃型腺癌临床诊治中国专家共识(2023年版)[J]. 中国实用妇科与产科杂志, 2023, 39(6): 617-625. |
| Gynecologic Oncology Group of Chinese Association of Obstetricians and Gynecologists. Chinese expert consensus on clinical diagnosis and treatment of gastric-type endocervical adenocarcinoma (2023 edition)[J]. Chin J Pract Gynecol Obstet, 2023, 39(6): 617-625. | |
| [15] |
STOEHR A, NANN D, STAEBLER A, et al. Difficulties in diagnosis of a minimal deviation adenocarcinoma of uterine cervix diagnosed postoperatively: brief communication and literature review[J]. Arch Gynecol Obstet, 2019, 300(4): 1029-1043.
doi: 10.1007/s00404-019-05286-7 pmid: 31529365 |
| [16] |
SAIDA T, SAKATA A, TANAKA Y O, et al. Clinical and MRI characteristics of uterine cervical adenocarcinoma: its variants and mimics[J]. Korean J Radiol, 2019, 20(3): 364-377.
doi: 10.3348/kjr.2018.0458 pmid: 30799567 |
| [17] | OMORI M, KONDO T, TAGAYA H, et al. Utility of imaging modalities for predicting carcinogenesis in lobular endocervical glandular hyperplasia[J]. PLoS One, 2019, 14(8): e0221088. |
| [18] |
SCHREUDER S M, LENSING R, STOKER J, et al. Monitoring treatment response in patients undergoing chemoradiotherapy for locally advanced uterine cervical cancer by additional diffusion-weighted imaging: a systematic review[J]. J Magn Reson Imaging, 2015, 42(3): 572-594.
doi: 10.1002/jmri.24784 pmid: 25346470 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
