Welcome to China Oncology,
China Oncology ›› 2022, Vol. 32 ›› Issue (2): 125-133.doi: 10.19401/j.cnki.1007-3639.2022.02.004
Previous Articles Next Articles
XU Hua1, LIU Ying1, ZHANG Yi1, WANG Tingliang1, WANG Tao1, HE Jinguang1, LUO Jie1, DONG Liping1, WANG Hairong1, DONG Jiasheng1, XU Yuanbing1,2( )
)
Received:2021-10-20
Revised:2022-01-20
Online:2022-02-28
Published:2022-03-08
Contact:
XU Yuanbing
E-mail:443430731@qq.com
Share article
CLC Number:
XU Hua, LIU Ying, ZHANG Yi, WANG Tingliang, WANG Tao, HE Jinguang, LUO Jie, DONG Liping, WANG Hairong, DONG Jiasheng, XU Yuanbing. Application of CT angiography in delayed DIEP flap breast reconstruction[J]. China Oncology, 2022, 32(2): 125-133.
Tab. 1
Comparison of baseline data between two groups"
| Factors | CTA group | US group | F/χ2 | P value |
|---|---|---|---|---|
| Age/year | 41.78±9.06 | 40.94±8.61 | 1.25 | 0.27 |
| BMI | 24.34±3.20 | 24.21±2.86 | 0.71 | 0.40 |
| Basic disease | 0.098 | 0.754 | ||
| With | 25 | 10 | ||
| Without | 181 | 82 | ||
| Chemotherapy | 0.281 | 0.596 | ||
| With | 158 | 69 | ||
| Without | 48 | 23 | ||
| Chest-wall radiotherapy | 0.001 | 0.977 | ||
| With | 72 | 32 | ||
| Without | 134 | 60 | ||
| Abdominal surgery | 0.264 | 0.608 | ||
| With | 82 | 36 | ||
| Without | 124 | 56 | ||
| Smoking | 0.017 | 0.895 | ||
| Yes | 4 | 2 | ||
| No | 202 | 90 | ||
| Blood supply of flap | 0.128 | 0.720 | ||
| Unipedicle | 85 | 40 | ||
| Bipedicle | 121 | 52 |
Tab. 2
Comparison of intraoperative and postoperative indicators between two groups"
| Indicators | CTA group | US group | F/χ2 | P value |
|---|---|---|---|---|
| Number of preoperative location perforations | 2.90±1.13 | 3.21±1.46 | 6.460 | 0.012 |
| Number of intraoperative choice perforations | 2.26±0.92 | 2.49±0.96 | 0.907 | 0.342 |
| Perforation choice time t/min | 9.14±3.38 | 26.73±6.54 | 49.420 | <0.001 |
| Perforation anatomy time t/min | 40.92±9.98 | 58.11±14.44 | 19.640 | <0.001 |
| Donor site flap acquisition time t/min | 50.05±10.94 | 84.80±15.44 | 15.560 | <0.001 |
| Flap weight m/g | 730.62±127.31 | 718.25±129.36 | 0.005 | 0.942 |
| Total operation time t/min | 294.20±68.51 | 328.74±68.69 | 0.058 | 0.809 |
| Abdominal incision infection | 0.199 | 0.656 | ||
| Yes | 3 | 2 | ||
| No | 203 | 90 | ||
| Fat necrosis | 0.404 | 0.525 | ||
| Yes | 6 | 4 | ||
| No | 200 | 88 | ||
| Secondary surgical exploration | 11.501 | <0.001 | ||
| Yes | 6 | 12 | ||
| No | 200 | 80 | ||
| Complete flap necrosis | ||||
| Yes | 0 | 2 | 0.095 | |
| No | 206 | 90 |
Tab. 3
Stratification analysis according to the history of abdominal surgery between two groups"
| Groups | Perforation anatomy time t/min | P value | Total operation time t/min | P value |
|---|---|---|---|---|
| ① CTA+NAS | 32.06±7.96 | 0.023a | 288.46±58.34 | 0.040e |
| ② CTA+AS | 42.36±10.06 | <0.001b | 300.06±60.29 | 0.018f |
| ③ US+NAS | 50.98±13.02 | <0.001c | 304.78±64.58 | 0.248g |
| ④ US+AS | 68.30±15.08 | 0.012d | 332.03±70.28 | 0.014h |
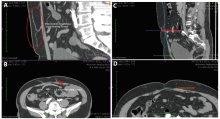
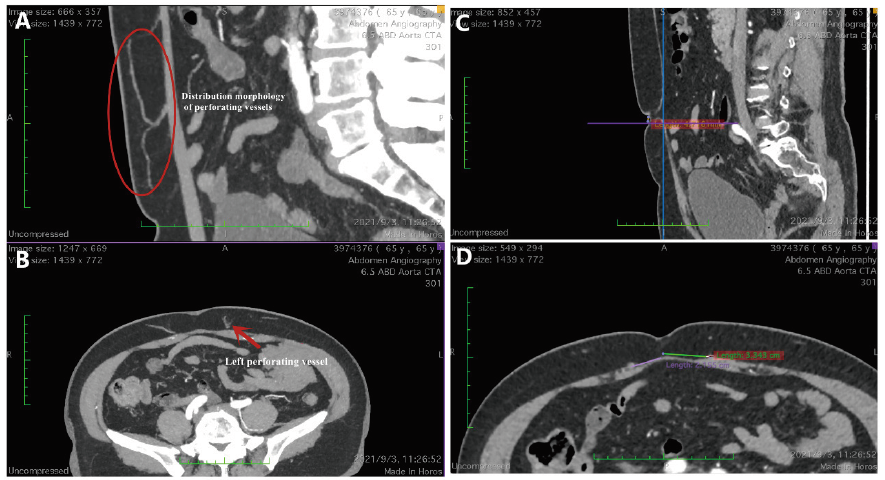
Fig. 4
CTA images of perforator vesselsA: The left perforator was in the shape direction of the flap; B: The exit point of the left perforator flap; C: Vertical distance between sagittal perforating branches and the center of the umbilicus; D: Vertical distance between left and right perforating branches and the center of the umbilicus."
| [1] | LIU C,, ZHAO Z Y,, GU X, et al.Establishment and verification of a bagged-trees-based model for prediction of sentinel lymph node metastasis for early breast cancer patients[J]. Front Oncol, 2019, 9: 282. |
| [2] | YANG B L,, REN G S,, SONG E W, et al.Current status and factors influencing surgical options for breast cancer in China: a nationwide cross-sectional survey of 110 hospitals[J]. Oncologist, 2020, 25(10): e1473-e1480. |
| [3] | HADDOCK N T,, DUMESTRE D O,, TEOTIA S S.Efficiency in DIEP flap breast reconstruction: the real benefit of computed tomographic angiography imaging[J]. Plast Reconstr Surg, 2020, 146(4): 719-723. |
| [4] | SMIT J M,, DIMOPOULOU A,, LISS A G, et al.Preoperative CT angiography reduces surgery time in perforator flap reconstruction[J]. J Plast Reconstr Aesthet Surg, 2009, 62(9): 1112-1117. |
| [5] | TONG W M,, DIXON R,, EKIS H, et al.The impact of preoperative CT angiography on breast reconstruction with abdominal perforator flaps[J]. Ann Plast Surg, 2012, 68(5): 525-530. |
| [6] | SANDBERG L J.Tracing: a simple interpretation method for the DIEP flap CT angiography to help operative decision-making[J]. Plast Reconstr Surg Glob Open, 2020, 8(11): e3218. |
| [7] | ROZEN W M,, BHULLAR H K,, HUNTER-SMITH D.How to assess a CTA of the abdomen to plan an autologous breast reconstruction[J]. Gland Surg, 2019, 8(Suppl 4): S291-S296. |
| [8] | 谢庆平,, 穆籣,, 刘元波, 等. 腹壁下动脉穿支皮瓣专家共识[J]. 中华显微外科杂志, 2020, 43(5): 417-423. |
| XIE Q P,, MU L,, LIU Y B, et al.Expert consensus of inferior epigastric artery perforator flap[J]. Chin J Microsurg, 2020, 43(5): 417-423. | |
| [9] | WILKINS E G,, HAMILL J B,, KIM H M, et al.Complications in postmastectomy breast reconstruction: one-year outcomes of the mastectomy reconstruction outcomes consortium (MROC) study[J]. Ann Surg, 2018, 267(1): 164-170. |
| [10] | 郝爽,, 吴炅. 腹壁下深血管穿支皮瓣在乳房重建应用中的技术难点与要点[J]. 中华内分泌外科杂志, 2021, 15(5): 449-453. |
| HE S,, WU J.Technical difficulties and key points of subabdominal deep vascular perforator flap in breast reconstruction[J]. Chin J Endocrine surg, 2021, 15(5): 449-453. | |
| [11] | DELLACROCE F J,, DELLACROCE H C,, BLUM C A, et al.Myth-busting the DIEP flap and an introduction to the abdominal perforator exchange (APEX) breast reconstruction technique: a single-surgeon retrospective review[J]. Plast Reconstr Surg, 2019, 143(4): 992-1008. |
| [12] | 刘元波,, 朱珊,, 臧梦青, 等. 穿支皮瓣研究领域的新技术、新方法[J]. 中华整形外科杂志, 2019, 35(9): 835-846. |
| LIU Y B,, ZHU S,, ZANG M Q, et al.New methods and technologies in the field of perforator flap studies[J]. Chin J Plast Surg, 2019(9): 835-846. | |
| [13] | KHAN U D,, MILLER J G.Reliability of handheld Doppler in planning local perforator-based flaps for extremities[J]. Aesthetic Plast Surg, 2007, 31(5): 521-525. |
| [14] | KEHRER A,, HEIDEKRUEGER P I,, LONIC D, et al.High-resolution ultrasound-guided perforator mapping and characterization by the microsurgeon in lower limb reconstruction[J]. J Reconstr Microsurg, 2021, 37(1): 75-82. |
| [15] | SU W J,, LU L G,, LAZZERI D, et al.Contrast-enhanced ultrasound combined with three-dimensional reconstruction in preoperative perforator flap planning[J]. Plast Reconstr Surg, 2013, 131(1): 80-93. |
| [16] | ROZEN W M,, GARCIA-TUTOR E,, ALONSO-BURGOS A, et al.Planning and optimising DIEP flaps with virtual surgery: the Navarra experience[J]. J Plast Reconstr Aesthet Surg, 2010, 63(2): 289-297. |
| [17] | MASIA J,, CLAVERO J A,, LARRAÑAGA J R, et al. Multidetector-row computed tomography in the planning of abdominal perforator flaps[J]. J Plast Reconstr Aesthet Surg, 2006, 59(6): 594-599. |
| [18] | TEUNIS T,, VAN VOSS M R H,, KON M, et al. CT-angiography prior to DIEP flap breast reconstruction: a systematic review and meta-analysis[J]. Microsurgery, 2013, 33(6): 496-502. |
| [19] | WAGNER R D,, DOVAL A F,, MEHRA N V, et al.Incidental findings in CT and MR angiography for preoperative planning in DIEP flap breast reconstruction[J]. Plast Reconstr Surg Glob Open, 2020, 8(10): e3159. |
| [20] | WEUM S,, MERCER J B,, DE WEERD L.Evaluation of dynamic infrared thermography as an alternative to CT angiography for perforator mapping in breast reconstruction: a clinical study[J]. BMC Med Imaging, 2016, 16(1): 43. |
| [21] | THIMMAPPA N,, BHAT A P,, BISHOP K, et al.Preoperative cross-sectional mapping for deep inferior epigastric and profunda artery perforator flaps[J]. Cardiovasc Diagn Ther, 2019, 9(Suppl 1): S131-S142. |
| [22] | SUFFEE T,, PIGNEUR F,, RAHMOUNI A, et al.Best choice of perforator vessel in autologous breast reconstruction: virtual reality navigation vs radiologist analysis. A prospective study[J]. J Plast Surg Hand Surg, 2015, 49(6): 333-338. |
| [23] | PARRETT B M,, CATERSON S A,, TOBIAS A M, et al.DIEP flaps in women with abdominal scars: are complication rates affected?[J]. Plast Reconstr Surg, 2008, 121(5): 1527-1531. |
| [24] | ROOSTAEIAN J,, YOON A P,, SANCHEZ I S, et al.The effect of prior abdominal surgery on abdominally based free flaps in breast reconstruction[J]. Plast Reconstr Surg, 2014, 133(3): 247e-255e. |
| [25] | MALHOTRA A,, CHHAYA N,, NSIAH-SARBENG P, et al.CT-guided deep inferior epigastric perforator (DIEP) flap localization: better for the patient, the surgeon, and the hospital[J]. Clin Radiol, 2013, 68(2): 131-138. |
| [26] | 彭文,, 吕春柳,, 周波, 等. 术前CT血管造影在腹壁下动脉穿支皮瓣乳房再造的应用现状和展望[J]. 中国修复重建外科杂志, 2020, 34(7): 927-931. |
| PENG W,, LÜ C L,, ZHOU B, et al.Application and prospect of preoperative computed tomographic angiography in deep inferior epigastric artery perforator flap for breast reconstruction[J]. Chin J Reparative Reconstr Surg, 2020, 34(7): 927-931. |
| [1] | XU Rui, WANG Zehao, WU Jiong. Advances in the role of tumor-associated neutrophils in the development of breast cancer [J]. China Oncology, 2024, 34(9): 881-889. |
| [2] | CAO Xiaoshan, YANG Beibei, CONG Binbin, LIU Hong. The progress of treatment for brain metastases of triple-negative breast cancer [J]. China Oncology, 2024, 34(8): 777-784. |
| [3] | ZHANG Jian. Clinical consideration of two key questions in assessing menopausal status of female breast cancer patients [J]. China Oncology, 2024, 34(7): 619-627. |
| [4] | JIANG Dan, SONG Guoqing, WANG Xiaodan. Study on the mechanism of mitochondrial dysfunction and CPT1A/ERK signal transduction pathway regulating malignant behavior in breast cancer [J]. China Oncology, 2024, 34(7): 650-658. |
| [5] | DONG Jianqiao, LI Kunyan, LI Jing, WANG Bin, WANG Yanhong, JIA Hongyan. A study on mechanism of SIRT3 inducing endocrine drug resistance in breast cancer via deacetylating YME1L1 [J]. China Oncology, 2024, 34(6): 537-547. |
| [6] | HAO Xian, HUANG Jianjun, YANG Wenxiu, LIU Jinting, ZHANG Junhong, LUO Yubei, LI Qing, WANG Dahong, GAO Yuwei, TAN Fuyun, BO Li, ZHENG Yu, WANG Rong, FENG Jianglong, LI Jing, ZHAO Chunhua, DOU Xiaowei. Establishment of primary breast cancer cell line as new model for drug screening and basic research [J]. China Oncology, 2024, 34(6): 561-570. |
| [7] | Committee of Breast Cancer Society, China Anti-Cancer Association. Expert consensus on clinical applications of ovarian function suppression for Chinese women with early breast cancer (2024 edition) [J]. China Oncology, 2024, 34(3): 316-333. |
| [8] | ZHANG Qi, XIU Bingqiu, WU Jiong. Progress of important clinical research of breast cancer in China in 2023 [J]. China Oncology, 2024, 34(2): 135-142. |
| [9] | ZHANG Siyuan, JIANG Zefei. Important research progress in clinical practice for advanced breast cancer in 2023 [J]. China Oncology, 2024, 34(2): 143-150. |
| [10] | WANG Zhaobu, LI Xing, YU Xinmiao, JIN Feng. Important research progress in clinical practice for early breast cancer in 2023 [J]. China Oncology, 2024, 34(2): 151-160. |
| [11] | LUO Yang, SUN Tao, SHAO Zhimin, CUI Jiuwei, PAN Yueyin, ZHANG Qingyuan, CHENG Ying, LI huiping, YANG Yan, YE Changsheng, YU Guohua, WANG Jingfen, LIU Yunjiang, LIU Xinlan, ZHOU Yuhong, BAI Yuju, GU Yuanting, WANG Xiaojia, XU Binghe, SONG Lihua. Efficacy, metabolic characteristics, safety and immunogenicity of AK-HER2 compared with reference trastuzumab in patients with metastatic HER2-positive breast cancer: a multicenter, randomized, double-blind phase Ⅲ equivalence trial [J]. China Oncology, 2024, 34(2): 161-175. |
| [12] | CHEN Yuanxiang, YU Tao, YANG Shiyu, ZENG Tao, WEI Lan, ZHANG Yan. KDM4A promotes the migration and invasion of breast cancer cell line MDA-MB-231 by downregulating BMP9 [J]. China Oncology, 2024, 34(2): 176-184. |
| [13] | HU Xiaoyu, CAI Yuwen, YE Fugui, SHAO Zhimin, HU Weigang, YU Keda. Impact of BRCA1/2 germline mutation on the incidence of second primary cancer following postoperative radiotherapy in patients with triple-negative breast cancer [J]. China Oncology, 2024, 34(2): 185-190. |
| [14] | ZHANG Siwei, MA Ding, JIANG Yizhou, SHAO Zhimin. “Subtype-precise” therapy leads diagnostic and therapeutic innovations: a new pattern for precision treatment of breast cancer [J]. China Oncology, 2024, 34(11): 1045-1052. |
| [15] | OUYANG Fei, WANG Yang, CHEN Yu, PEI Guoqing, WANG Ling, ZHANG Yang, SHI Lei. Construction of the prediction model of breast cancer bone metastasis based on machine learning [J]. China Oncology, 2024, 34(10): 903-914. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
