Welcome to China Oncology,
China Oncology ›› 2024, Vol. 34 ›› Issue (7): 650-658.doi: 10.19401/j.cnki.1007-3639.2024.07.004
• Article • Previous Articles Next Articles
JIANG Dan1( ), SONG Guoqing1(
), SONG Guoqing1( ), WANG Xiaodan2
), WANG Xiaodan2
Received:2023-10-30
Revised:2024-06-15
Online:2024-07-30
Published:2024-08-08
Contact:
SONG Guoqing
Share article
CLC Number:
JIANG Dan, SONG Guoqing, WANG Xiaodan. Study on the mechanism of mitochondrial dysfunction and CPT1A/ERK signal transduction pathway regulating malignant behavior in breast cancer[J]. China Oncology, 2024, 34(7): 650-658.

Fig. 1
Abnormal expression of CPT1A in breast cancer tissue promotes tumor metastasis A, B: The expression of CPT1A mRNA in breast cancer tissues (n=1 085), normal breast tissues (n=291) and breast cancer tissues with different stages was analyzed by GEPIA. C: Using TCGA GEPIA to generate Kaplan-Meier diagram of breast cancer patients. The data of 1 069 breast cancer patients were divided into two groups according to the median percentile of CPT1A expression. D, E: Western blot representation and quantitative analysis of the expression level of CPT1A after overexpression. F, G: Transwell were used to determine the invasive ability of breast cancer cells expressing CPT1A or negative control vector. H, I: Western blot representation and quantitative analysis of the expression level of CPT1A after shRNA knockdown. J, K: Transwell were used to determine the invasive ability of breast cancer cells or negative control cells after CPT1A knock-down. *: P<0.05, compared with normal breast tissues; ***: P<0.001, compared with NC group."
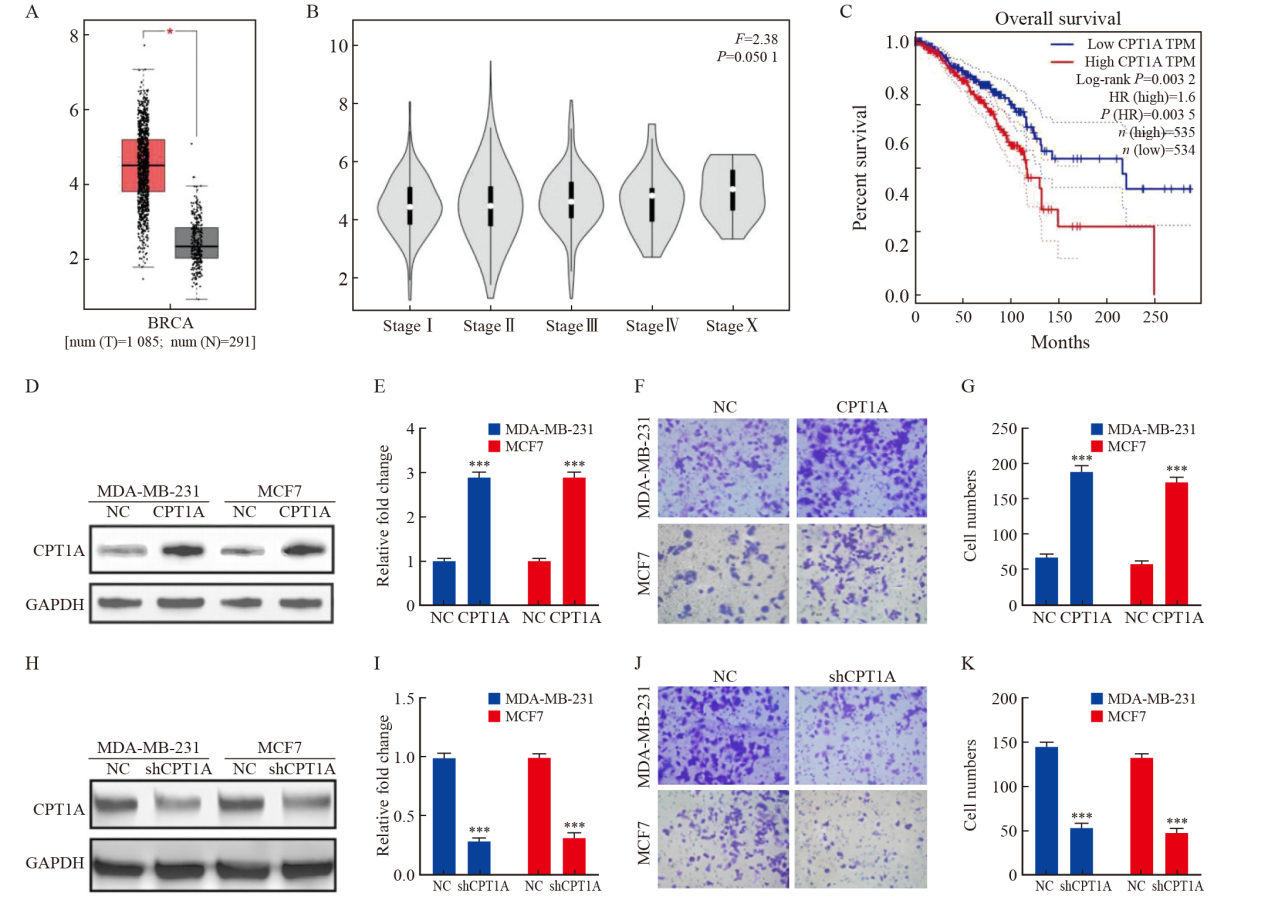
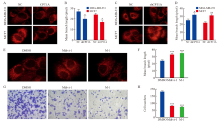
Fig. 2
CPT1A promotes breast cancer cell metastasis by regulating mitochondrial division A, B: Mitotracker living cell mitochondrial imaging and average mitochondrial branch length of cells overexpressing CPT1A or negative control. C, D: Mitotracker living cell mitochondrial imaging and average mitochondrial branch length of shRNA knock-down or negative control cells. E, F: Mitotracker mitochondrial imaging and average mitochondrial branching length of CPT1A overexpressing MDA-MB-231 cells treated with Mdivi-1 and M-1. G, H: Transwell was used to determine the invasive ability of CPT1A cells overexpressed MDA-MB-231 treated with Mdivi-1 and M-1. *: P<0.05, compared with NC group; **: P<0.01, compared with NC group; ***: P<0.001, compared with DMSO group."
Fig. 3
CPT1A activates PGC-1α through ERK1/2 A: Antibody array scanning of MDA-MB-231 cells overexpressing CPT1A. B, C: Western blot analysis and quantitative analysis of ERK1/2-PGC-1α expression in MDA-MB-231 cells over-expressing CPT1A. D, E: Western blot analysis and quantitative analysis of ERK1/2-PGC-1α expression in MDA-MB-231 cells treated with different doses of PD325901 for 8 h. *: P<0.05, compared with 0 nmol/L group; **: P<0.01, compared with NC group or 0 nmol/L group; ***: P<0.001, compared with NC group or 0 nmol/L group."
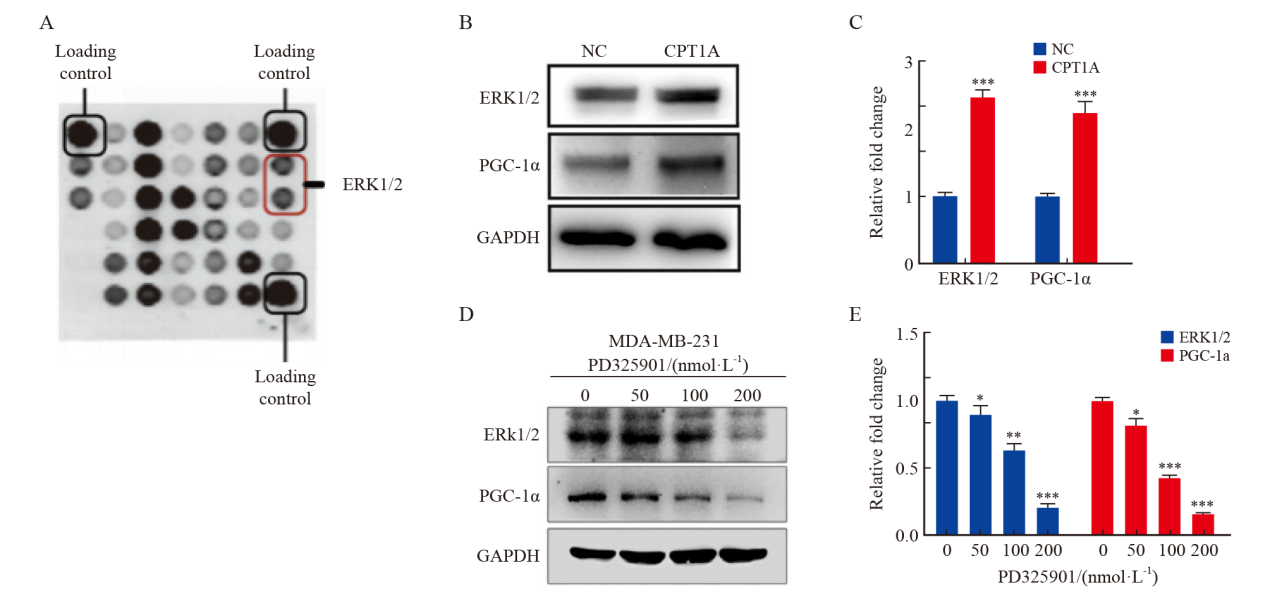
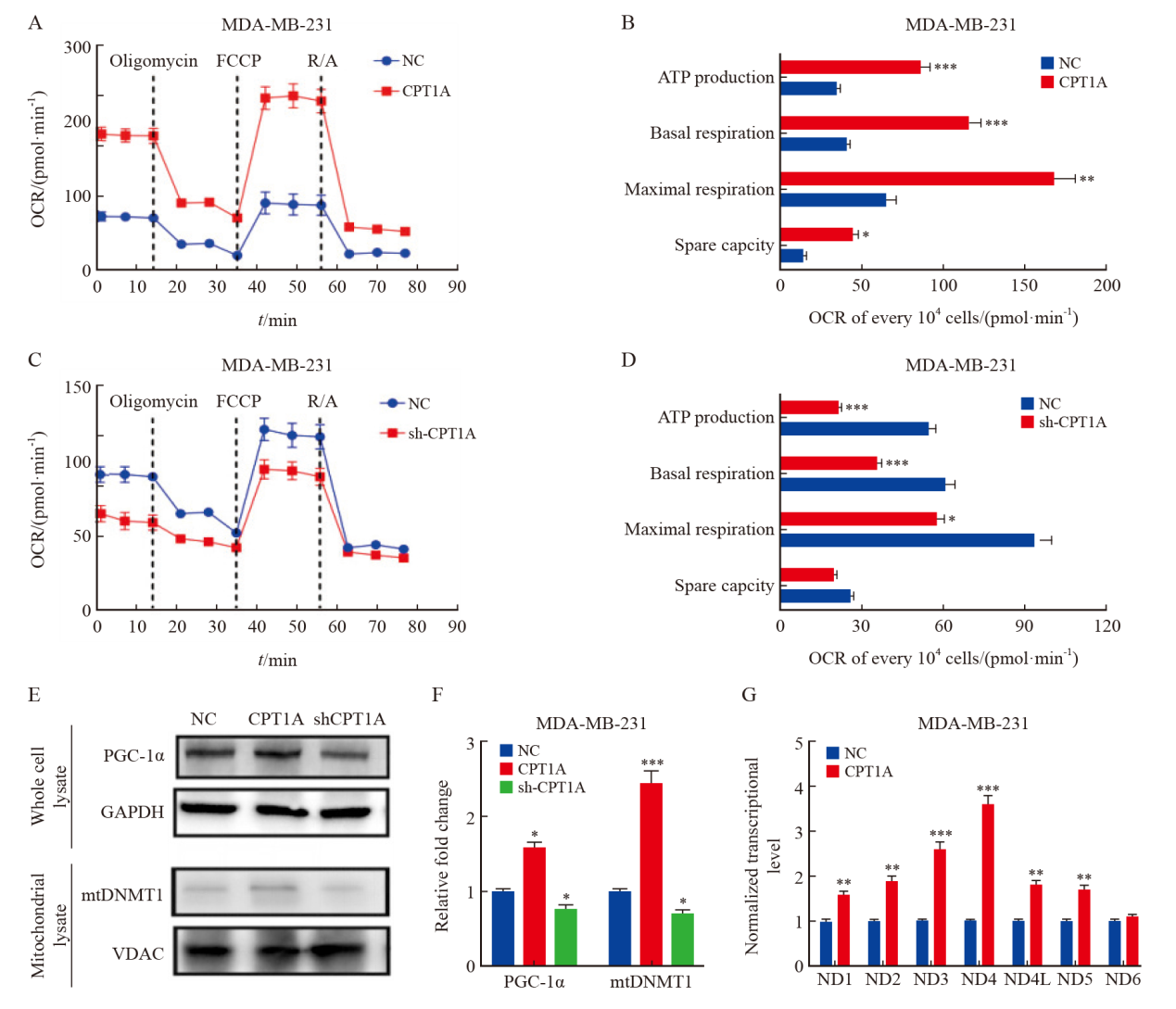
Fig. 4
CPT1A promotes mitochondrial oxidative phosphorylation A, B: Real-time OCR tracing of MDA-MB-231 cells overexpressing CPT1A and negative control and statistics of respiratory parameters. C, D: Real-time OCR tracing of MDA-MB-231 cells with CPT1A knockdown and negative control and statistics of respiratory parameters. E, F: Western blot analysis of the expression and quantitative analysis of PGC-1α and mitochondrial DNMT1 in MDA-MB-231 cells that overexpressed CPT1A and knocked down CPT1A. G: The expression level of mitochondrial DNA coding gene was measured by Taqman assay, and the data was standardized to 18s rRNA. *: P<0.05, compared with NC group; **: P<0.01, compared with NC group; ***: P<0.001, compared with NC group."
| [1] | GIAQUINTO A N, SUNG H, MILLER K D, et al. Breast cancer statistics, 2022[J]. CA Cancer J Clin, 2022, 72(6): 524-541. |
| [2] | XIA C F, DONG X S, LI H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants[J]. Chin Med J, 2022, 135(5): 584-590. |
| [3] | GALIANDRO F, AGNES S, MOSCHETTA G, et al. Prognostic factors in patients with breast cancer liver metastases undergoing liver resection: systematic review and meta-analysis[J]. Cancers, 2022, 14(7): 1691. |
| [4] | KOTECHA R, TONSE R, RUBENS M, et al. Systematic review and meta-analysis of breast cancer brain metastasis and primary tumor receptor expression discordance[J]. Neurooncol Adv, 2021, 3(1): vdab010. |
| [5] | VONA R, MILEO A M, MATARRESE P. Microtubule-based mitochondrial dynamics as a valuable therapeutic target in cancer[J]. Cancers, 2021, 13(22): 5812. |
| [6] | KUMAR H, GUPTA N V, JAIN R, et al. A review of biological targets and therapeutic approaches in the management of triple-negative breast cancer[J]. J Adv Res, 2023, 54: 271-292. |
| [7] | JIANG N, XING B Z, PENG R, et al. Inhibition of Cpt1a alleviates oxidative stress-induced chondrocyte senescence via regulating mitochondrial dysfunction and activating mitophagy[J]. Mech Ageing Dev, 2022, 205: 111688. |
| [8] |
SAVUKAITYTĖ A, BARTNYKAITĖ A, BEKAMPYTĖ J, et al. DDIT4 downregulation by siRNA approach increases the activity of proteins regulating fatty acid metabolism upon aspirin treatment in human breast cancer cells[J]. Curr Issues Mol Biol, 2023, 45(6): 4665-4674.
doi: 10.3390/cimb45060296 pmid: 37367045 |
| [9] | JOSHI M, KIM J, D’ALESSANDRO A, et al. CPT1A over-expression increases reactive oxygen species in the mitochondria and promotes antioxidant defenses in prostate cancer[J]. Cancers, 2020, 12(11): 3431. |
| [10] |
DAS M, GIANNOUDIS A, SHARMA V. The role of CPT1A as a biomarker of breast cancer progression: a bioinformatic approach[J]. Sci Rep, 2022, 12(1): 16441.
doi: 10.1038/s41598-022-20585-x pmid: 36180554 |
| [11] | ZHANG W, DU X F, LIU B, et al. Engineering supramolecular nanomedicine for targeted near infrared-triggered mitochondrial dysfunction to potentiate cisplatin for efficient chemophototherapy[J]. ACS Nano, 2022, 16(1): 1421-1435. |
| [12] | FORTE M, SCHIRONE L, AMERI P, et al. The role of mitochondrial dynamics in cardiovascular diseases[J]. Br J Pharmacol, 2021, 178(10): 2060-2076. |
| [13] | YOU Y, MURAOKA S, JEDRYCHOWSKI M P, et al. Human neural cell type-specificextracellular vesicle proteome defines disease-related molecules associated with activated astrocytes in Alzheimer’s disease brain[J]. J Extracell Vesicles, 2022, 11(1): e12183. |
| [14] | ANSARI M I, BANO N, KAINAT K M, et al. Bisphenol A exposure induces metastatic aggression in low metastatic MCF-7 cells via PGC-1α mediated mitochondrial biogenesis and epithelial-mesenchymal plasticity[J]. Life Sci, 2022, 302: 120649. |
| [15] | MIDDLETON P, VERGIS N. Mitochondrial dysfunction and liver disease: role, relevance, and potential for therapeutic modulation[J]. Therap Adv Gastroenterol, 2021, 14: 17562848211031394. |
| [16] |
LIU Y E, SHI Y F. Mitochondria as a target in cancer treatment[J]. MedComm, 2020, 1(2): 129-139.
doi: 10.1002/mco2.16 pmid: 34766113 |
| [17] | LEE K M, GILTNANE J M, BALKO J M, et al. MYC and MCL1 cooperatively promote chemotherapy-resistant breast cancer stem cells via regulation of mitochondrial oxidative phosphorylation[J]. Cell Metab, 2017, 26(4): 633-647. e7. |
| [18] | PRAHARAJ P P, PATRO B S, BHUTIA S K. Dysregulation of mitophagy and mitochondrial homeostasis in cancer stem cells: novel mechanism for anti-cancer stem cell-targeted cancer therapy[J]. Br J Pharmacol, 2022, 179(22): 5015-5035. |
| [19] | ZHANG L, SUN L, WANG L R, et al. Mitochondrial division inhibitor (mdivi-1) inhibits proliferation and epithelial-mesenchymal transition via the NF-κB pathway in thyroid cancer cells[J]. Toxicol In Vitro, 2023, 88: 105552. |
| [20] |
RANA A, OLIVEIRA M P, KHAMOUI A V, et al. Promoting Drp1-mediated mitochondrial fission in midlife prolongs healthy lifespan of drosophila melanogaster[J]. Nat Commun, 2017, 8(1): 448.
doi: 10.1038/s41467-017-00525-4 pmid: 28878259 |
| [21] | HU N, CHEN X M, CHEN C C, et al. Exploring the role of esketamine in alleviating depressive symptoms in mice via the PGC-1α/irisin/ERK1/2 signaling pathway[J]. Sci Rep, 2023, 13(1): 16611. |
| [22] |
HUANG K Y, LIU Z Y, XIE Z L, et al. HIGD2A silencing impairs hepatocellular carcinoma growth via inhibiting mitochondrial function and the MAPK/ERK pathway[J]. J Transl Med, 2023, 21(1): 253.
doi: 10.1186/s12967-023-04105-7 pmid: 37041638 |
| [23] |
LIU J F, NING L. Protective role of emodin in rats with post-myocardial infarction heart failure and influence on extracellular signal-regulated kinase pathway[J]. Bioengineered, 2021, 12(2): 10246-10253.
doi: 10.1080/21655979.2021.1983977 pmid: 34839778 |
| [24] | LAURIN K M, COUTU-BEAUDRY K, SALAZAR A, et al. Low expression of PGC-1β and other mitochondrial biogenesis modulators in melanoma is associated with growth arrest and the induction of an immunosuppressive gene expression program dependent on MEK and IRF-1[J]. Cancer Lett, 2022, 541: 215738. |
| [25] | ASL E R, AMINI M, NAJAFI S, et al. Interplay between MAPK/ERK signaling pathway and microRNAs: a crucial mechanism regulating cancer cell metabolism and tumor progression[J]. Life Sci, 2021, 278: 119499. |
| [1] | XU Rui, WANG Zehao, WU Jiong. Advances in the role of tumor-associated neutrophils in the development of breast cancer [J]. China Oncology, 2024, 34(9): 881-889. |
| [2] | CAO Xiaoshan, YANG Beibei, CONG Binbin, LIU Hong. The progress of treatment for brain metastases of triple-negative breast cancer [J]. China Oncology, 2024, 34(8): 777-784. |
| [3] | ZHANG Jian. Clinical consideration of two key questions in assessing menopausal status of female breast cancer patients [J]. China Oncology, 2024, 34(7): 619-627. |
| [4] | DONG Jianqiao, LI Kunyan, LI Jing, WANG Bin, WANG Yanhong, JIA Hongyan. A study on mechanism of SIRT3 inducing endocrine drug resistance in breast cancer via deacetylating YME1L1 [J]. China Oncology, 2024, 34(6): 537-547. |
| [5] | HAO Xian, HUANG Jianjun, YANG Wenxiu, LIU Jinting, ZHANG Junhong, LUO Yubei, LI Qing, WANG Dahong, GAO Yuwei, TAN Fuyun, BO Li, ZHENG Yu, WANG Rong, FENG Jianglong, LI Jing, ZHAO Chunhua, DOU Xiaowei. Establishment of primary breast cancer cell line as new model for drug screening and basic research [J]. China Oncology, 2024, 34(6): 561-570. |
| [6] | Committee of Breast Cancer Society, China Anti-Cancer Association. Expert consensus on clinical applications of ovarian function suppression for Chinese women with early breast cancer (2024 edition) [J]. China Oncology, 2024, 34(3): 316-333. |
| [7] | ZHANG Qi, XIU Bingqiu, WU Jiong. Progress of important clinical research of breast cancer in China in 2023 [J]. China Oncology, 2024, 34(2): 135-142. |
| [8] | ZHANG Siyuan, JIANG Zefei. Important research progress in clinical practice for advanced breast cancer in 2023 [J]. China Oncology, 2024, 34(2): 143-150. |
| [9] | WANG Zhaobu, LI Xing, YU Xinmiao, JIN Feng. Important research progress in clinical practice for early breast cancer in 2023 [J]. China Oncology, 2024, 34(2): 151-160. |
| [10] | LUO Yang, SUN Tao, SHAO Zhimin, CUI Jiuwei, PAN Yueyin, ZHANG Qingyuan, CHENG Ying, LI huiping, YANG Yan, YE Changsheng, YU Guohua, WANG Jingfen, LIU Yunjiang, LIU Xinlan, ZHOU Yuhong, BAI Yuju, GU Yuanting, WANG Xiaojia, XU Binghe, SONG Lihua. Efficacy, metabolic characteristics, safety and immunogenicity of AK-HER2 compared with reference trastuzumab in patients with metastatic HER2-positive breast cancer: a multicenter, randomized, double-blind phase Ⅲ equivalence trial [J]. China Oncology, 2024, 34(2): 161-175. |
| [11] | CHEN Yuanxiang, YU Tao, YANG Shiyu, ZENG Tao, WEI Lan, ZHANG Yan. KDM4A promotes the migration and invasion of breast cancer cell line MDA-MB-231 by downregulating BMP9 [J]. China Oncology, 2024, 34(2): 176-184. |
| [12] | HU Xiaoyu, CAI Yuwen, YE Fugui, SHAO Zhimin, HU Weigang, YU Keda. Impact of BRCA1/2 germline mutation on the incidence of second primary cancer following postoperative radiotherapy in patients with triple-negative breast cancer [J]. China Oncology, 2024, 34(2): 185-190. |
| [13] | ZHANG Siwei, MA Ding, JIANG Yizhou, SHAO Zhimin. “Subtype-precise” therapy leads diagnostic and therapeutic innovations: a new pattern for precision treatment of breast cancer [J]. China Oncology, 2024, 34(11): 1045-1052. |
| [14] | OUYANG Fei, WANG Yang, CHEN Yu, PEI Guoqing, WANG Ling, ZHANG Yang, SHI Lei. Construction of the prediction model of breast cancer bone metastasis based on machine learning [J]. China Oncology, 2024, 34(10): 903-914. |
| [15] | ZHAO Junxiu, ZHU Yi, SONG Xiaoyu, ZHE Chao, XIAO Yuhan, LIU Yunduo, LI Linhai, XIAO Bin. Circ-0007766 acts as a miR-1972 sponge to promote breast cancer cell migration and invasion via upregulation of HER2 [J]. China Oncology, 2024, 34(10): 915-930. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
