Welcome to China Oncology,
China Oncology ›› 2024, Vol. 34 ›› Issue (6): 581-589.doi: 10.19401/j.cnki.1007-3639.2024.06.006
• Article • Previous Articles Next Articles
JIANG Tiaoyan1,2( ), JIA Tianying2, ZHANG Qin2(
), JIA Tianying2, ZHANG Qin2( )(
)( )
)
Received:2024-04-23
Revised:2024-06-18
Online:2024-06-30
Published:2024-07-16
Share article
CLC Number:
JIANG Tiaoyan, JIA Tianying, ZHANG Qin. Contrast-enhanced computed tomography-based radiomics models for the risk categorization of thymoma[J]. China Oncology, 2024, 34(6): 581-589.
Tab. 1
Clinical characteristics of patients"
| Characteristics | Low-risk thymomas (n=273) | High-risk thymomas (n=205) | P value |
|---|---|---|---|
| Gender n (%) | |||
| Male | 122 (44.69) | 107 (52.2) | 0.10 |
| Female | 151 (55.31) | 98 (47.8) | |
| Age/year | |||
| x±s | 54.5±10.8 | 50.9±13.7 | 0.01 |
| Maximal diameter D/cm | |||
| x±s | 6.18±2.97 | 6.07±2.57 | 0.98 |
| Comorbidity n(%) | |||
| Present | 9 (3.3) | 36 (17.56) | <0.001 |
| Absent | 264 (96.70) | 169 (82.44) | |
| Masaoka-Koga stage n (%) | |||
| Ⅰ | 110 (40.29) | 28 (13.66) | <0.001 |
| Ⅱ | 148 (54.21) | 117 (57.07) | |
| Ⅲ | 15 (5.49) | 60 (29.27) |
Tab. 2
Comparison of clinical characteristics between training and test set"
| Characteristics | Training set (n=382) | Test set (n=96) | P value |
|---|---|---|---|
| Gender | |||
| Male | 218 (57.07) | 55 (57.29) | 0.97 |
| Female | 164 (42.93) | 41 (42.71) | |
| Age/year | |||
| x±s | 52.9±12.3 | 53.1±12.0 | 0.66 |
| Maximal diameter D/cm | |||
| x±s | 6.03±2.74 | 6.36±3.09 | 0.38 |
| Concomitant disease n (%) | |||
| Present | 35 (9.16) | 10 (10.42) | 0.71 |
| Absent | 347 (90.84) | 86 (89.58) | |
| Masaoka-Koga stage n(%) | |||
| Ⅰ | 111 (29.06) | 27 (28.13) | 0.91 |
| Ⅱ | 211 (55.24) | 54 (56.25) | |
| Ⅲ | 60 (15.71) | 15 (15.63) | |
| Risk category n (%) | |||
| Low risk | 218 (57.07) | 55 (57.29) | 0.97 |
| High risk | 164 (42.93) | 41 (42.71) |
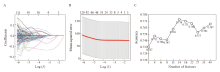
Fig. 2
Feature selection using the LASSO regression algorithm and the performance of the baseline logistic regression model A: The LASSO coefficients of the 581 features; B: Mean square error with respect to log(λ). The average binominal deviance values for each model at a given λ were indicated by the dashed red curve; C: Mean accuracy of the baseline logistic model at a given number of features. Two regional maxima were found at 4 and 14 features."
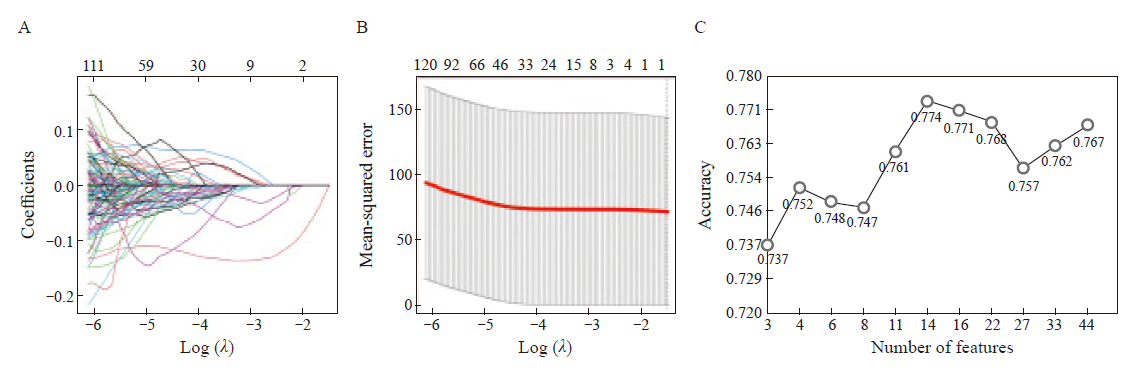
Fig. 3
ROC curves of risk group classification models on the training and test sets A: ROC curve of the QDA model based on clinical features with an area under the ROC curve (AUC) of 0.652 (95% CI: 0.596-0.707) and 0.666 (95% CI: 0.554-0.777) on the training and test sets. The sensitivity and specificity at the best decision point were 0.341 and 0.945 on the test set. B: LDA model using fourteen radiomics features with an AUC of 0.849 on the training set and 0.800 on the test set. Sensitivity and specificity were 0.707 and 0.782 on the test set. C: QDA model using four radiomics features with an AUC of 0.831 on both the training and test sets. Sensitivity and specificity were 0.756 and 0.818, respectively, on the test set. D: Logistic regression model based on clinical and radiomic features with an AUC of 0.830 (95% CI: 0.788-0.871) and 0.850 (95% CI: 0.773-0.927) on the training and test set, respectively. Sensitivity and specificity were 0.829 and 0.764 on the test set. E: Comparison of the ROC curves of the three models."
Tab. 3
Model performance measured on the test set"
| Data | AUC | 95% CI | P value | Sensitivity | Specificity | Accuracy |
|---|---|---|---|---|---|---|
| Clinical | 0.666 | 0.554-0.777 | 0.0028 | 0.341 | 0.945 | 0.688 |
| CECT-1* | 0.800 | 0.711-0.890 | <0.001 | 0.707 | 0.782 | 0.750 |
| CECT-2** | 0.831 | 0.747-0.914 | <0.001 | 0.756 | 0.818 | 0.792 |
| Combined*** | 0.850 | 0.773-0.927 | <0.001 | 0.829 | 0.764 | 0.792 |
| [1] |
PRIOLA A M, PRIOLA S M, CARDINALE L, et al. The anterior mediastinum: diseases[J]. Radiol Med, 2006, 111(3): 312-342.
doi: 10.1007/s11547-006-0032-5 pmid: 16683081 |
| [2] |
MARX A, CHAN J K, COINDRE J M, et al. The 2015 World Health Organization classification of tumors of the thymus: continuity and changes[J]. J Thorac Oncol, 2015, 10(10): 1383-1395.
doi: 10.1097/JTO.0000000000000654 pmid: 26295375 |
| [3] |
CHEN G, MARX A, CHEN W H, et al. New WHO histologic classification predicts prognosis of thymic epithelial tumors: a clinicopathologic study of 200 thymoma cases from China[J]. Cancer, 2002, 95(2): 420-429.
doi: 10.1002/cncr.10665 pmid: 12124843 |
| [4] | GIRARD N, RUFFINI E, MARX A, et al. ESMO Guidelines Committee. Thymic epithelial tumours: ESMO clinical practice guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2015, 26(Suppl 5): v40-55. |
| [5] |
SCORSETTI M, LEO F, TRAMA A, D'ANGELILLO R, et al. Thymoma and thymic carcinomas[J]. Crit Rev Oncol Hematol, 2016, 99: 332-350.
doi: 10.1016/j.critrevonc.2016.01.012 pmid: 26818050 |
| [6] | VENUTA F, RENDINA E A, LONGO F, et al. Long-term outcome after multimodality treatment for stage Ⅲ thymic tumors[J]. Ann Thorac Surg, 2003, 76(6): 1866-1872; discussion1872. |
| [7] | VENUTA F, RENDINA E A, PESCARMONA E O, et al. Multimodality treatment of thymoma: a prospective study[J]. Ann Thorac Surg, 1997, 64(6): 1585-1591; discussion: 1591-1592. |
| [8] |
OTANI Y, YOSHIDA I, ISHIKAWA S, et al. Neoadjuvant intra-arterial infusion chemotherapy for invasive thymoma[J]. Oncol Rep, 1997, 4(1): 23-25.
doi: 10.3892/or.4.1.23 pmid: 21590005 |
| [9] | JEONG Y J, LEE K S, KIM J, et al. Does CT of thymic epithelial tumors enable us to differentiate histologic types and predict prognosis?[J]. AJR Am J Roentgenol, 2004, 183(2): 283-289. |
| [10] | LIU J, YIN P, WANG S C, et al. CT-based radiomics signatures for predicting the risk categorization of thymic epithelial tumors[J]. Front Oncol, 2021, 11: 628534. |
| [11] |
FEDOROV A, BEICHEL R, KALPATHY-CRAMER J, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network[J]. Magn Reson Imaging, 2012, 30(9): 1323-1341.
doi: 10.1016/j.mri.2012.05.001 pmid: 22770690 |
| [12] | FRIEDMAN J, HASTIE T, TIBSHIRANI R. Regularization paths for generalized linear models via coordinate descent[J]. J Statistical Software, 33(1): 1-22. |
| [13] | BISCHL B, LANG M, KOTTHOFF L, et al. MLR: machine learning in R[J]. J Machine Learning Res, 2016, 17(1): 5938-5942. |
| [14] |
ABDEL RAZEK A A, KHAIRY M, NADA N. Diffusion-weighted MR imaging in thymic epithelial tumors: correlation with world health organization classification and clinical staging[J]. Radiology, 2014, 273(1): 268-275.
doi: 10.1148/radiol.14131643 pmid: 24877982 |
| [15] | XIAO G, HU Y C, REN J L, et al. MR imaging of thymomas: a combined radiomics nomogram to predict histologic types[J]. Eur Radiol, 2021, 31(1): 447-457. |
| [16] | WANG X H, SUN W, LIANG H Y, et al. Radiomics signatures of computed tomography imaging for predicting risk categorization and clinical stage of thymomas[J]. Biomed Res Int, 2019, 2019: 3616852. |
| [17] | XIAO G, RONG W C, HU Y C, et al. MRI radiomics analysis for predicting the pathologic classification and TNM staging of thymic epithelial tumors: a pilot studyB[J]. AJR Am J Roentgenol, 2020, 214(2): 328-340. |
| [18] | DONG W T, XIONG S T, LEI P G, et al. Application of a combined radiomics nomogram based on CE-CT in the preoperative prediction of thymomas risk categorization[J]. Front Oncol, 2022, 12: 944005. |
| [19] | YU C, LI T, YANG X, ZHANG R, et al. Contrast-enhanced CT-based radiomics model for differentiating risk subgroups of thymic epithelial tumors[J]. BMC Med Imaging, 2022, 22(1): 37. |
| [20] |
LIU W, WANG W, ZHANG H Y, et al. Development and validation of multi-omics thymoma risk classification model based on transfer learning[J]. J Digit Imaging, 2023, 36(5): 2015-2024.
doi: 10.1007/s10278-023-00855-4 pmid: 37268842 |
| [21] | SHANG L, WANG F, GAO Y, et al. Machine-learning classifiers based on non-enhanced computed tomography radiomics to differentiate anterior mediastinal cysts from thymomas and low-risk from high-risk thymomas: a multi-center study[J]. Front Oncol, 2022, 12: 1043163. |
| [22] | KAYI CANGIR A, ORHAN K, KAHYA Y, et al. CT imaging-based machine learning model: a potential modality for predicting low-risk and high-risk groups of thymoma: "impact of surgical modality choice"[J]. World J Surg Oncol, 2021, 19(1): 147. |
| [23] |
OZKAN E, ORHAN K, SOYDAL C, et al. Combined clinical and specific positron emission tomography/computed tomography-based radiomic features and machine-learning model in prediction of thymoma risk groups[J]. Nucl Med Commun, 2022, 43(5): 529-539.
doi: 10.1097/MNM.0000000000001547 pmid: 35234213 |
| [24] | RAJAMOHAN N, GOYAL A, KANDASAMY D, et al. CT texture analysis in evaluation of thymic tumors and thymic hyperplasia: correlation with the international thymic malignancy interest group (ITMIG) stage and WHO grade[J]. Br J Radiol, 2021, 94(1128): 20210583. |
| [25] |
IANNARELLI A, SACCONI B, TOMEI F, et al. Analysis of CT features and quantitative texture analysis in patients with thymic tumors: correlation with grading and staging[J]. Radiol Med, 2018, 123(5): 345-350.
doi: 10.1007/s11547-017-0845-4 pmid: 29307077 |
| [26] | FENG X L, WANG S Z, CHEN H H, et al. Optimizing the radiomics-machine-learning model based on non-contrast enhanced CT for the simplified risk categorization of thymic epithelial tumors: a large cohort retrospective study[J]. Lung Cancer, 2022, 166: 150-160. |
| [27] | NAKAJO M, TAKEDA A, KATSUKI A, et al. The efficacy of 18F-FDG-PET-based radiomic and deep-learning features using a machine-learning approach to predict the pathological risk subtypes of thymic epithelial tumors[J]. Br J Radiol, 2022, 95(1134): 20211050. |
| [28] |
MAHMOUDI S, GRUENEWALD L D, EICHLER K, et al. Multiparametric evaluation of radiomics features and dual-energy CT iodine maps for discrimination and outcome prediction of thymic masses[J]. Acad Radiol, 2023, 30(12): 3010-3021.
doi: 10.1016/j.acra.2023.03.034 pmid: 37105804 |
| [1] | HUANG Haozhe, CHEN Hong, ZHENG Dezhong, CHEN Chao, WANG Ying, XU Lichao, WANG Yaohui, HE Xinhong, YANG Yuanyuan, LI Wentao. A CT-based radiomics nomogram for predicting local tumor progression of colorectal cancer lung metastases treated with radiofrequency ablation [J]. China Oncology, 2024, 34(9): 857-872. |
| [2] | PAN Jian, YE Dingwei, ZHU Yao, WANG Beihe. Correlation analysis of PSMA PET/CT-derived parameters and circulating tumor DNA features in patients with hormone-sensitive prostate cancer [J]. China Oncology, 2024, 34(7): 680-685. |
| [3] | WU Hongji, WANG Haixia, WANG Ling, LUO Xiaogang, ZOU Dongling. Application progress and challenges of artificial intelligence in organoid research [J]. China Oncology, 2024, 34(2): 210-219. |
| [4] | OUYANG Fei, WANG Yang, CHEN Yu, PEI Guoqing, WANG Ling, ZHANG Yang, SHI Lei. Construction of the prediction model of breast cancer bone metastasis based on machine learning [J]. China Oncology, 2024, 34(10): 903-914. |
| [5] | LIU Wei, XIE Tiansong, CHEN Lei, ZHANG Zehua, ZHOU Zhengrong. Investigating the value of dual-layer spectral detector CT in distinguishing resectable pancreatic ductal adenocarcinoma from mass-forming chronic pancreatitis [J]. China Oncology, 2024, 34(1): 67-73. |
| [6] | YANG Ziyi, GU Bingxin, XU Xiaoping, SONG Shaoli. Comparison of 18F-FDG and 68Ga-FAPI PET/CT in the diagnosis of lung metastasis in different malignant tumors [J]. China Oncology, 2023, 33(9): 829-833. |
| [7] | ZHOU Bingni, LIU Xiaohang, GU Bingxin, ZHOU Liangping, GU Yajia. The value of mpMRI combined with 99mTc-PSMA SPECT/CT in the detection of significant residual prostate cancer after neoadjuvant androgen deprivation therapy [J]. China Oncology, 2022, 32(2): 134-141. |
| [8] | XU Wenhao, TIAN Xi, Aihetaimujiang·Anwaier , QU Yuanyuan, SHI Guohai, ZHANG Hailiang, YE Dingwei. A systematic review of current advancements of artificial intelligence in genitourinary cancers [J]. China Oncology, 2022, 32(1): 68-74. |
| [9] | YANG Yanju, ZHONG Yang, HU Weigang, GAO Dadi, ZHAO Jun. Effects of CT-RED calibration curves of different simulators on dose distribution of tumor target and organs at risk [J]. China Oncology, 2021, 31(9): 828-837. |
| [10] | LUO Rong , HU Peian , XIE Tiansong , ZHANG Zehua , ZHOU Liangping , ZHOU Zhengrong , CHEN Lei . The correlation of imaging, clinical features and pathology of myxoid fibrosarcoma [J]. China Oncology, 2021, 31(8): 734-739. |
| [11] | HU Guannan , CHEN Lei , ZHOU Liangping , ZHOU Zhengrong . A case report of pulmonary malignant melanoma complicated with lung adenocarcinoma and literature review [J]. China Oncology, 2021, 31(7): 647-650. |
| [12] | YIN Zhihai, WANG Juanqi, MENG Yiran, XU Qing, YANG Zhaozhi. Investigation of patient characteristics associated with setup errors in intensity-modulated radiotherapy after breast-conserving surgery [J]. China Oncology, 2021, 31(3): 198-202. |
| [13] | LI Zeng , WU Yi , CHEN Zhuzhong , CHEN Li , LIAO Hong , MAO Dun , XIAO Yingming , XIE Hongping , LI Xiuli , YANG Shengke , ZHOU Shukui , ZHONG Lei , LU Hao , CHEN Yongji . The value of 18 F-PSMA-1007 PET/CT in the early diagnosis and clinical treatment of patients with biochemical recurrence after radical prostatectomy [J]. China Oncology, 2021, 31(11): 1081-1087. |
| [14] | REN Caiyue, WANG Shengping, ZHANG Shengjian, PENG Weijun. The value of MSCT signs combined with texture analysis in preoperatively predicting WHO simplified pathological classification of thymic epithelial tumors [J]. China Oncology, 2020, 30(6): 468-474. |
| [15] | WU Ziyi, WANG Yan, MENG Yiran, XU Qing. Comparison of the application of cone-beam CT and Catalyst TM system in image-guided radiotherapy [J]. China Oncology, 2020, 30(12): 1031-1034. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
