Welcome to China Oncology,
China Oncology ›› 2025, Vol. 35 ›› Issue (2): 228-236.doi: 10.19401/j.cnki.1007-3639.2025.02.010
• Specialist's Article • Previous Articles Next Articles
LU Yongjin1,2( ), SHI Zhiqiang1, LI Tong3, WANG Yongsheng1, QIU Pengfei1,2(
), SHI Zhiqiang1, LI Tong3, WANG Yongsheng1, QIU Pengfei1,2( )
)
Received:2024-12-27
Revised:2025-01-21
Online:2025-02-28
Published:2025-03-19
Supported by:Share article
CLC Number:
LU Yongjin, SHI Zhiqiang, LI Tong, WANG Yongsheng, QIU Pengfei. Retrospective study on regional lymph node radiotherapy after axillary dissection exemption in breast cancer patients with sentinel lymph node positive status[J]. China Oncology, 2025, 35(2): 228-236.
Tab. 1
Basic characteristics of the patient"
| RNI (n=186) | No-RNI (n=170) | P value | RNI (n=186) | No-RNI (n=170) | P value | |||
|---|---|---|---|---|---|---|---|---|
| Age/year | 0.093 | Vascular invasion | 0.098 | |||||
| Median | 47 (30-75) | 49 (27-75) | Yes | 59 (31.7%) | 40 (23.5%) | |||
| BMI | 0.173 | No | 127 (68.3%) | 130 (76.5%) | ||||
| Median | 24.24 (16.73-39.79) | 24.59 (17.22-38.87) | Estrogen receptor | 0.438 | ||||
| Menopause status | 0.828 | Negative | 28 (15.1%) | 20 (11.8%) | ||||
| Premenopausal | 116 (62.4%) | 104 (61.2%) | Positive | 158 (84.9%) | 150 (88.2%) | |||
| Postmenopausal | 70 (37.6%) | 66 (38.8%) | Progesterone receptor | 0.428 | ||||
| Laterality | 0.168 | Negative | 41 (22.0%) | 31 (18.2%) | ||||
| Left | 103 (55.4%) | 81 (47.6%) | Positive | 145 (78.0%) | 139 (81.8%) | |||
| Right | 83 (44.6%) | 89 (52.4%) | HER-2 | 0.143 | ||||
| Tumor location | 0.116 | Negative | 152 (81.7%) | 149 (87.6%) | ||||
| Lateral | 116 (62.4%) | 120 (70.6%) | Positive | 34 (18.3%) | 21 (12.4%) | |||
| Central/medial | 70 (37.6%) | 50 (29.4%) | Positive number of SLN | 0.006 | ||||
| Tumour size D/cm | 0.043 | 1 | 136 (73.1%) | 147 (86.5%) | ||||
| ≤2.0 | 101 (54.3%) | 112 (65.9%) | 2 | 42 (22.6%) | 20 (11.8%) | |||
| 2.0<D≤5.0 | 80 (43.0%) | 57 (33.5%) | 3 | 8 (4.3%) | 3 (1.8%) | |||
| >5.0 | 5 (2.7%) | 1(0.6%) | Type of surgery | <0.001 | ||||
| Histological type | 0.299 | TM | 133 (71.5%) | 35 (20.6%) | ||||
| IDC | 176 (94.6%) | 156 (91.8%) | BCS | 53 (28.5%) | 135 (79.4%) | |||
| Others | 10 (5.4%) | 14 (8.2%) | ||||||
| Histologic grade | 0.139 | |||||||
| Ⅰ | 2 (1.1%) | 2 (1.2%) | ||||||
| Ⅱ | 127 (68.3%) | 104 (61.2%) | ||||||
| Ⅲ | 51 (27.4%) | 49 (28.8%) | ||||||
| NA | 6 (3.2%) | 15 (8.8%) |
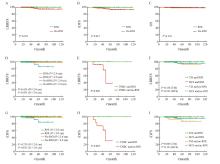
Fig. 2
Kaplan-Meier curves for survival analysis of breast cancer patients based on receipt of RNI The Kaplan-Meier curves illustrated LRRFS, iDFS, and OS for the patients. The first row presented the Kaplan-Meier curves for LRRFS (A), iDFS (B), and OS (C) comparing the RNI group (green) and the no-RNI group (red) in all patients. The second and third rows showed exploratory subgroup analyses of LRRFS and iDFS for different patient subgroups. D-G: Tumor size subgroups (R≤2 cm/RNI: Green; R>2 cm/RNI: Red; R≤ 2 cm/no-RNI: Orange; R>2 cm/no-RNI: Blue). E-H: Kaplan-Meier LRRFS and iDFS for triple-negative breast cancer (TNBC) patients (RNI: Green; no-RNI: Red). F, I: Surgical approach subgroups (TM/RNI: Green; BCS/RNI: Red; TM/no-RNI: Orange; BCS/no-RNI: Blue)."

| [1] | 李培, 吴炅. 中国乳腺癌外科治疗现状和新趋势[J]. 中国肿瘤临床, 2022, 49(22): 1151-1155. |
| LI P, WU J. Current status and new trends of surgical treatment for breast cancer in China[J]. Chin J Clin Oncol, 2022, 49(22): 1151-1155. | |
| [2] |
GIULIANO A E, KIRGAN D M, GUENTHER J M, et al. Lymphatic mapping and sentinel lymphadenectomy for breast cancer[J]. Ann Surg, 1994, 220(3): 391-398;discussion, 398-401.
doi: 10.1097/00000658-199409000-00015 pmid: 8092905 |
| [3] |
POODT I G M, SPRONK P E R, VUGTS G, et al. Trends on axillary surgery in nondistant metastatic breast cancer patients treated between 2011 and 2015: a Dutch population-based study in the ACOSOG-Z0011 and AMAROS era[J]. Ann Surg, 2018, 268(6): 1084-1090.
doi: 10.1097/SLA.0000000000002440 pmid: 28742702 |
| [4] | GARCIA-ETIENNE C A, MANSEL R E, TOMATIS M, et al. Trends in axillary lymph node dissection for early-stage breast cancer in Europe: impact of evidence on practice[J]. Breast, 2019, 45: 89-96. |
| [5] |
DONKER M, VAN TIENHOVEN G, STRAVER M E, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial[J]. Lancet Oncol, 2014, 15(12): 1303-1310.
doi: 10.1016/S1470-2045(14)70460-7 pmid: 25439688 |
| [6] | GIULIANO A E, BALLMAN K V, MCCALL L, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (alliance) randomized clinical trial[J]. JAMA, 2017, 318(10): 918-926. |
| [7] |
GALIMBERTI V, COLE B F, VIALE G, et al. Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23-01): 10-year follow-up of a randomised, controlled phase 3 trial[J]. Lancet Oncol, 2018, 19(10): 1385-1393.
doi: S1470-2045(18)30380-2 pmid: 30196031 |
| [8] | GIULIANO A E, HUNT K K, BALLMAN K V, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial[J]. JAMA, 2011, 305(6): 569-575. |
| [9] |
JAGSI R, CHADHA M, MONI J, et al. Radiation field design in the ACOSOG Z0011 (alliance) trial[J]. J Clin Oncol, 2014, 32(32): 3600-3606.
doi: 10.1200/JCO.2014.56.5838 pmid: 25135994 |
| [10] | BARTELS S A L, DONKER M, PONCET C, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer: 10-year results of the randomized controlled EORTC 10981-22023 AMAROS trial[J]. J Clin Oncol, 2023, 41(12): 2159-2165. |
| [11] | DE BONIFACE J, TVEDSKOV T F, RYDÉN L, et al. Omitting axillary dissection in breast cancer with sentinel-node metastases[J]. N Engl J Med, 2024, 390(13): 1163-1175. |
| [12] | 袁芊芊, 侯晋轩, 苏科华, 等. 基于上肢淋巴引流的乳腺癌术后水肿风险因素分析[J]. 中华普通外科杂志, 2021, 36(8): 579-584. |
| YUAN Q Q, HOU J X, SU K H, et al. Risk factors analysis of breast cancer-related lymphedema based on the proportion of the arm lymph flow above and below the axillary vein[J]. Chin J Gen Surg, 2021, 36(8): 579-584. | |
| [13] | 毕钊, 王永胜, 邱鹏飞. 2024版NCCN乳腺癌临床实践指南更新解读[J]. 中国肿瘤外科杂志, 2024, 16(5): 417-422. |
| BI Z, WANG Y S, QIU P F. Update and interpretation of NCCN clinical practice guidelines for breast cancer in 2024 edition[J]. Chin J Surg Oncol, 2024, 16(5): 417-422. | |
| [14] | 杨成林, 李建彬, 王玮. 乳腺癌术后放疗与全身系统治疗的顺序选择[J]. 中华放射医学与防护杂志, 2021, 41(10): 790-795. |
| YANG C L, LI J B, WANG W. Sequence selection of postoperative radiotherapy and systemic treatment for breast cancer patients[J]. Chin J Radiol Med Prot, 2021, 41(10): 790-795. | |
| [15] |
毕钊, 王永胜. 1-2枚前哨淋巴结阳性早期乳腺癌患者治疗策略降阶梯新理念[J]. 中国癌症杂志, 2023, 33(6): 560-565.
doi: 10.19401/j.cnki.1007-3639.2023.06.002 |
| BI Z, WANG Y S. New concept of de-escalation management strategy in breast cancer patients with 1-2 positive sentinel lymph nodes[J]. China Oncol, 2023, 33(6): 560-565. | |
| [16] | SÁVOLT Á, PÉLEY G, POLGÁR C, et al. Eight-year follow up result of the OTOASOR trial: the optimal treatment of the axilla-surgery or radiotherapy after positive sentinel lymph node biopsy in early-stage breast cancer a randomized, single centre, phase Ⅲ, non-inferiority trial[J]. Eur J Surg Oncol EJSO, 2017, 43(4): 672-679. |
| [17] |
KIM B K, PARK B W, HUR M H, et al. Omission of axillary lymph node dissection in patients who underwent total mastectomy with 1 or 2 metastatic lymph nodes[J]. Ann Surg Treat Res, 2020, 98(6): 283-290.
doi: 10.4174/astr.2020.98.6.283 pmid: 32528907 |
| [18] | GAO W Q, LU S S, ZENG Y F, et al. Axilla lymph node dissection can be safely omitted in patients with 1-2 positive sentinel nodes receiving mastectomy: a large multi-institutional study and a systemic meta-analysis[J]. Breast Cancer Res Treat, 2022, 196(1): 129-141. |
| [19] |
FITZSULLIVAN E, BASSETT R L, KUERER H M, et al. Outcomes of sentinel lymph node-positive breast cancer patients treated with mastectomy without axillary therapy[J]. Ann Surg Oncol, 2017, 24(3): 652-659.
doi: 10.1245/s10434-016-5605-5 pmid: 27822630 |
| [20] | TINTERRI C, GENTILE D, GATZEMEIER W, et al. Preservation of axillary lymph nodes compared with complete dissection in T1-2 breast cancer patients presenting one or two metastatic sentinel lymph nodes: the SINODAR-ONE multicenter randomized clinical trial[J]. Ann Surg Oncol, 2022, 29(9): 5732-5744. |
| [21] | GOYAL A, BRUCE MANN G, FALLOWFIELD L, et al. POSNOC-positive sentinel node: adjuvant therapy alone versus adjuvant therapy plus clearance or axillary radiotherapy: a randomised controlled trial of axillary treatment in women with early-stage breast cancer who have metastases in one or two sentinel nodes[J]. BMJ Open, 2021, 11(12): e054365. |
| [22] | WHELAN T J, OLIVOTTO I A, PARULEKAR W R, et al. Regional nodal irradiation in early-stage breast cancer[J]. N Engl J Med, 2015, 373(4): 307-316. |
| [23] | POORTMANS P M, WELTENS C, FORTPIED C, et al. Internal mammary and medial supraclavicular lymph node chain irradiation in stage Ⅰ-Ⅲ breast cancer (EORTC 22922/10925): 15-year results of a randomised, phase 3 trial[J]. Lancet Oncol, 2020, 21(12): 1602-1610. |
| [24] | EBCTCG (Early Breast Cancer Trialists' Collaborative Group). Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8 135 women in 22 randomised trials[J]. Lancet, 2014, 383(9935): 2127-2135. |
| [25] | ALKNER S, DE BONIFACE J, LUNDSTEDT D, et al. Protocol for the T-REX-trial: tailored regional external beam radiotherapy in clinically node-negative breast cancer patients with 1-2 sentinel node macrometastases-an open, multicentre, randomised non-inferiority phase 3 trial[J]. BMJ Open, 2023, 13(9): e075543. |
| [26] | SIT D, LALANI N, CHAN E, et al. Association between regional nodal irradiation and breast cancer recurrence-free interval for patients with low-risk, node-positive breast cancer[J]. Int J Radiat Oncol Biol Phys, 2022, 112(4): 861-869. |
| [27] | 焦得闯, 朱久俊, 乔江华, 等. 前哨淋巴结1-2枚转移的早期乳腺癌患者非前哨淋巴结转移状态分析[J]. 中华普通外科杂志, 2018, 33(7): 571-574. |
| JIAO D C, ZHU J J, QIAO J H, et al. Nonsentinel lymph nodal status in 1-2 sentinel lymph node positive early breast cancer patients[J]. Chin J Gen Surg, 2018, 33(7): 571-574. | |
| [28] |
YANG Z B, LAN X W, HUANG Z, et al. Development and external validation of a nomogram to predict four or more positive nodes in breast cancer patients with one to three positive sentinel lymph nodes[J]. Breast, 2020, 53: 143-151.
doi: S0960-9776(20)30154-5 pmid: 32823167 |
| [29] |
SPECHT M C, KATTAN M W, GONEN M, et al. Predicting nonsentinel node status after positive sentinel lymph biopsy for breast cancer: clinicians versus nomogram[J]. Ann Surg Oncol, 2005, 12(8): 654-659.
pmid: 16021535 |
| [30] |
VAN ZEE K J, MANASSEH D E, BEVILACQUA J L B, et al. A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy[J]. Ann Surg Oncol, 2003, 10(10): 1140-1151.
doi: 10.1245/aso.2003.03.015 pmid: 14654469 |
| [1] | LU Yufeng, WANG Han, XIE Yifan, JIANG Yizhou, SHAO Zhimin. Significant fundamental translational research on breast cancer in China: progress and prospects [J]. China Oncology, 2025, 35(2): 143-153. |
| [2] | LIN Jialin, WANG Wenna, XU Binghe. Current status and future perspectives of antibody-drug conjugates in breast cancer therapy [J]. China Oncology, 2025, 35(2): 154-166. |
| [3] | YANG Xin, SHI Qianfeng, LIU Qiang. Progress of important clinical research on breast cancer in China in 2024 [J]. China Oncology, 2025, 35(2): 167-175. |
| [4] | LI Xing, PENG Ziqi, YU Xinmiao, JIN Feng. Important research progress in clinical practice for early breast cancer in 2024 [J]. China Oncology, 2025, 35(2): 176-185. |
| [5] | WU Song, YUAN Yang, JIANG Zefei. Important clinical studies that changed the clinical practice of advanced breast cancer in 2024 [J]. China Oncology, 2025, 35(2): 186-194. |
| [6] | ZENG Cheng, WANG Yuanyi, WANG Jiani, MA Fei. Advances in immune checkpoint inhibitor therapy for breast cancer: research progress and future directions [J]. China Oncology, 2025, 35(2): 195-204. |
| [7] | LI Junjie. Progress and future prospects in local and systemic treatment of early breast cancer [J]. China Oncology, 2025, 35(2): 205-212. |
| [8] | WANG Qing, YU Yushuai, WANG Chenxi, JIANG Zirong, LI Jialu, TANG Shicong, SONG Chuangui. Current status and prospects of tertiary lymphoid structure heterogeneity in predicting response to neoadjuvant therapy and characterizing immune microenvironment in triple-negative breast cancer [J]. China Oncology, 2025, 35(2): 213-218. |
| [9] | CAI Shuyue, XIE Quan, ZHOU Yuxuan, LIU Qingzhu, QIU Ling, LIN Jianguo. Latest progress and prospect of NRP-1 targeted molecular probes for breast cancer diagnosis [J]. China Oncology, 2025, 35(2): 249-254. |
| [10] | XU Rui, WANG Zehao, WU Jiong. Advances in the role of tumor-associated neutrophils in the development of breast cancer [J]. China Oncology, 2024, 34(9): 881-889. |
| [11] | CAO Xiaoshan, YANG Beibei, CONG Binbin, LIU Hong. The progress of treatment for brain metastases of triple-negative breast cancer [J]. China Oncology, 2024, 34(8): 777-784. |
| [12] | ZHANG Jian. Clinical consideration of two key questions in assessing menopausal status of female breast cancer patients [J]. China Oncology, 2024, 34(7): 619-627. |
| [13] | JIANG Dan, SONG Guoqing, WANG Xiaodan. Study on the mechanism of mitochondrial dysfunction and CPT1A/ERK signal transduction pathway regulating malignant behavior in breast cancer [J]. China Oncology, 2024, 34(7): 650-658. |
| [14] | DONG Jianqiao, LI Kunyan, LI Jing, WANG Bin, WANG Yanhong, JIA Hongyan. A study on mechanism of SIRT3 inducing endocrine drug resistance in breast cancer via deacetylating YME1L1 [J]. China Oncology, 2024, 34(6): 537-547. |
| [15] | HAO Xian, HUANG Jianjun, YANG Wenxiu, LIU Jinting, ZHANG Junhong, LUO Yubei, LI Qing, WANG Dahong, GAO Yuwei, TAN Fuyun, BO Li, ZHENG Yu, WANG Rong, FENG Jianglong, LI Jing, ZHAO Chunhua, DOU Xiaowei. Establishment of primary breast cancer cell line as new model for drug screening and basic research [J]. China Oncology, 2024, 34(6): 561-570. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
