Welcome to China Oncology,
China Oncology ›› 2024, Vol. 34 ›› Issue (6): 527-536.doi: 10.19401/j.cnki.1007-3639.2024.06.001
• Article • Previous Articles Next Articles
WENG Junyong( ), YE Zilan, ZHANG Ruoxin, LIU Qi, LI Xinxiang(
), YE Zilan, ZHANG Ruoxin, LIU Qi, LI Xinxiang( )(
)( )
)
Received:2024-04-18
Revised:2024-06-10
Online:2024-06-30
Published:2024-07-16
Share article
CLC Number:
WENG Junyong, YE Zilan, ZHANG Ruoxin, LIU Qi, LI Xinxiang. Exploring the guiding role of the number of adverse pathological features in risk stratification for recurrence of stage Ⅰ-Ⅲ colorectal cancer: a retrospective cohort study of 9 875 cases[J]. China Oncology, 2024, 34(6): 527-536.
Tab. 1
Characteristics baseline of patients [n (%)]"
| Variables | Hr_0 group (n=4 509) | Hr_1 group (n=2 803) | Hr_2 group (n=1703) | Hr_3 group (n=655) | Hr_4 group (n=208) |
|---|---|---|---|---|---|
| Age/year* | 61 (15.0) | 60 (16.0) | 60 (16.0) | 60 (18.0) | 54 (22.5) |
| Gender | |||||
| Male | 2 701 (59.9) | 1 664 (59.4) | 973 (57.1) | 387 (59.1) | 134 (65.4) |
| Female | 1 808 (40.1) | 1 139 (40.1) | 730 (42.9) | 268 (40.9) | 71 (34.6)) |
| Histologic type | |||||
| Adenocarcinoma | 4 509 (100.0) | 2 538 (90.5) | 1 178 (69.2) | 428 (65.3) | 39 (19.0) |
| Mucinous | 0 (0.0) | 263 (9.4) | 494 (29.0) | 178 (27.2) | 92 (444.9) |
| Signet ring cell | 0 (0.0) | 2 (0.1) | 31 (1.8) | 49 (7.5) | 74 (36.1) |
| Differentiation | |||||
| Poor | 0 (0.0) | 512 (18.3) | 984 (57.8) | 591 (90.2) | 204 (99.5) |
| Moderate | 4 369 (96.9) | 2 254 (80.4) | 707 (41.5) | 63 (9.6) | 1 (0.5) |
| Well | 140 (3.1) | 37 (1.3) | 12 (0.7) | 1 (0.2) | 0 (0.0) |
| Perineural invasion | |||||
| Negative | 4 509 (100.0) | 1 922 (68.6) | 951 (55.8) | 169 (25.8) | 9 (4.4) |
| Positive | 0 (0.0) | 881 (31.4) | 752 (44.2) | 486 (74.2) | 196 (95.6) |
| Lymphovascular invasion | |||||
| Negative | 4 509 (100.0) | 1 979 (70.6) | 769 (45.2) | 115 (17.6) | 9 (4.4) |
| Positive | 0 (0.0) | 824 (29.4) | 934 (54.8) | 540 (82.4) | 196 (95.6) |
| pT stage | |||||
| T1/Tis | 419 (9.3) | 115 (4.1) | 26 (1.5) | 7 (1.1) | 1 (0.5) |
| T2 | 1 145 (25.4) | 439 (15.7) | 156 (9.2) | 31 (4.7) | 10 (4.9) |
| T3 | 1 290 (28.6) | 1 052 (37.5) | 731 (42.9) | 281 (42.9) | 74 (36.1) |
| T4 | 1 655 (36.7) | 1 197 (42.7) | 790 (46.4) | 336 (51.3) | 120 (58.5) |
| pN stage | |||||
| N0 | 3 369 (74.7) | 1 206 (43.0) | 498 (29.2) | 90 (13.7) | 1 (0.5) |
| N1 | 918 (20.4) | 876 (31.3) | 594 (34.9) | 184 (28.1) | 36 (17.6) |
| N2 | 222 (4.9) | 416 (14.8) | 431 (25.3) | 284 (43.4) | 113 (55.1) |
| Nx | 0 (0.0) | 305 (10.9) | 180 (10.6) | 97 (14.8) | 55 (26.8) |
| TNM | |||||
| 0-Ⅰ | 1 312 (29.1) | 234 (8.3) | 72 (4.2) | 12 (1.8) | 1 (0.5) |
| Ⅱ | 1 997 (44.3) | 958 (34.2) | 411 (24.1) | 75 (11.5) | 3 (1.4) |
| Ⅲ | 1 200 (26.6) | 1 306 (46.6) | 1 040 (61.1) | 471 (71.9) | 149 (71.6) |
| Unknown | 305 (10.9) | 305 (10.9) | 180 (10.6) | 97 (14.8) | 55 (26.4) |
| Position | |||||
| Rectum | 2 462 (54.6) | 1 336 (47.7) | 761 (44.7) | 319 (48.7) | 109 (53.2) |
| Left-sided colon | 1 023 (22.7) | 697 (24.9) | 406 (23.8) | 129 (19.7) | 39 (19.0) |
| Right-sided colon | 1 012 (22.4) | 765 (27.3) | 535 (31.4) | 206 (31.5) | 57 (27.8) |
| Unknown | 12 (0.3) | 5 (0.2) | 1 (0.1) | 1 (0.2) | 0 (0.0) |
| Resection margin | |||||
| Negative | 4 509 (100.0) | 2 787 (99.4) | 1 672 (98.2) | 631 (96.3) | 175 (85.4) |
| Positive | 0 (0.0) | 16 (0.6) | 31 (1.8) | 24 (3.7) | 30 (14.6) |
| Number of lymph node harvest | |||||
| <12 | 0 (0.0) | 305 (10.9) | 180 (10.6) | 97 (14.8) | 55 (26.8) |
| ≥12 | 4 509 (100.0) | 2 498 (89.1) | 1 523 (89.4) | 558 (85.2) | 150 (73.2) |
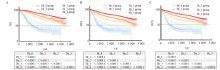
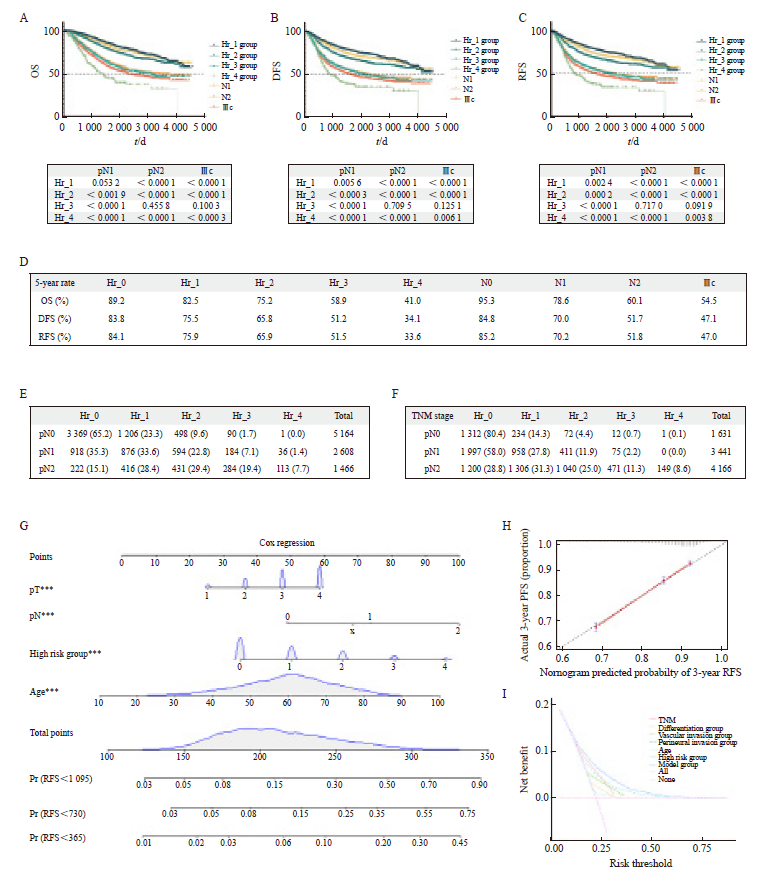
Fig. 2
Survival curves of different Hr groups A: OS survival curves and the results of comparisons between different Hr group categories; B: DFS survival curves and the results of comparisons between different Hr group categories; C: RFS survival curves and the results of comparisons between different Hr group categories. Bonferroni correction was applied, with P<0.005 indicating statistical significance."
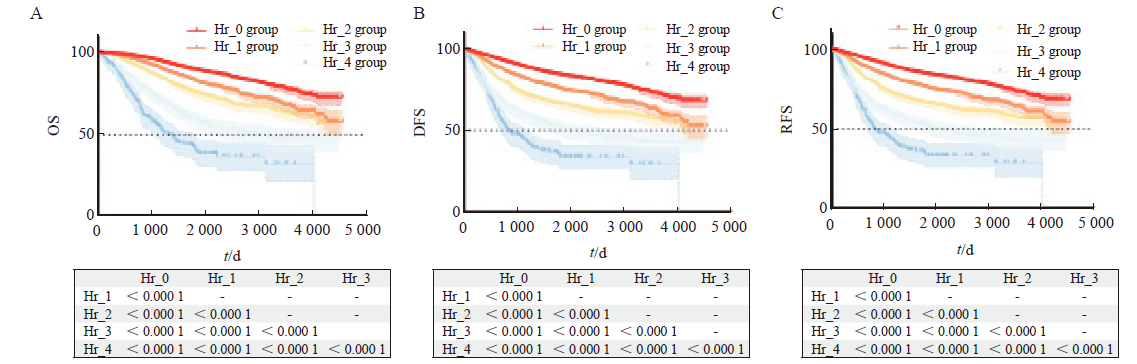
Fig. 3
Survival curves for different Hr groups in subgroup analysis for staging A-C: OS, DFS, and RFS survival curves for stage Ⅱ colorectal cancer patients in different Hr group categories, with Bonferroni correction applied, P<0.008 considered as statistically significant; D-F: OS, DFS, and RFS survival curves for stage Ⅲ colorectal cancer patients in different Hr group categories, with Bonferroni correction applied, P<0.005 considered as statistically significant."
Tab. 2
Multivariable regression analysis for OS, DFS and RFS"
| Item | OS | DFS | RFS | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | |||
| Age | 1.040 (1.036-1.045) | <0.000 1 | 1.022 (1.018-1.025) | <0.000 1 | 1.022 (1.018-1.026) | <0.000 1 | ||
| Hr_1 vs Hr_0 | 1.268 (1.110-1.450) | <0.000 1 | 1.254 (1.121-1.404) | <0.000 1 | 1.242 (1.109-1.391) | <0.000 1 | ||
| Hr_2 vs Hr_0 | 1.626 (1.403-1.884) | <0.000 1 | 1.620 (1.433-1.833) | <0.000 1 | 1.632 (1.443-1.847) | <0.000 1 | ||
| Hr_3 vs Hr_0 | 2.656 (2.225-3.171) | <0.000 1 | 2.288 (1.962-2.668) | <0.000 1 | 2.300 (1.972-2.682) | <0.000 1 | ||
| Hr_4 vs Hr_0 | 4.923 (3.908-6.201) | <0.000 1 | 3.517 (2. 850-4.340) | <0.000 1 | 3.603 (2.924-4.438) | <0.000 1 | ||
| pT3 vs pT1 | 1.693 (1.191-2.405) | 0.003 0 | 1.750 (1.323-2.315) | <0.000 1 | 1.872 (1.398-2.507) | <0.000 1 | ||
| pT4 vs pT1 | 2.108 (1.499-2.966) | <0.000 1 | 1.985 (1.510-2.609) | <0.000 1 | 2.161 (1.623-2.877) | <0.000 1 | ||
| pN1 vs pN0 | 1.691 (1.483-1.928) | <0.000 1 | 1.615 (1.449-1.800) | <0.000 1 | 1.643 (1.473-1. 832) | <0.000 1 | ||
| pN2 vs pN0 | 3.219 (2.795-3.708) | <0.000 1 | 2.701 (2.395-3.046) | <0.000 1 | 2.743 (2.431-3.096) | <0.000 1 | ||

Fig. 4
The potential clinical value of Hr group grouping A-C: OS, DFS, and RFS survival curves for different Hr groups, different pN stages, and stage Ⅲc were adjusted using Bonferroni, with P<0.004 2 indicating statistically significant differences; D: 5-year OS, 5-year DFS and 5-year RFS for different Hr group groups, different pN stages, and stage Ⅲc; E: Cross tabulation of Hr group grouping and pN staging; F: Cross tabulation of Hr group grouping and TNM staging; G: Column chart of RFS risks for 1, 2, and 3 years; H: Calibration curve of the 3-year RFS column chart model; I: The DCA curve of the recurrence risk model."
| [1] | HAN B F, ZHENG R S, ZENG H M, et al. Cancer incidence and mortality in China, 2022[J]. J Natl Cancer Cent, 2024, 4(1): 47-53. |
| [2] | KLINGBIEL D, SARIDAKI Z, ROTH A D, et al. Prognosis of stage Ⅱ and Ⅲ colon cancer treated with adjuvant 5-fluorouracil or FOLFIRI in relation to microsatellite status: results of the PETACC-3 trial[J]. Ann Oncol, 2015, 26(1): 126-132. |
| [3] | RIBIC C M, SARGENT D J, MOORE M J, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer[J]. N Engl J Med, 2003, 349(3): 247-257. |
| [4] |
SARGENT D J, MARSONI S, MONGES G, et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer[J]. J Clin Oncol, 2010, 28(20): 3219-3226.
doi: 10.1200/JCO.2009.27.1825 pmid: 20498393 |
| [5] | KIM J E, HONG Y S, KIM H J, et al. Defective mismatch repair status was not associated with DFS and OS in stage Ⅱ colon cancer treated with adjuvant chemotherapy[J]. Ann Surg Oncol, 2015, 22(Suppl 3): S630-S637. |
| [6] | BENSON A B, VENOOK A P, AL-HAWARY M M, et al. Colon cancer, version 2.2021, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2021, 19(3): 329-359. |
| [7] | 中国临床肿瘤学会指南工作委员会组织. 中国临床肿瘤学会(CSCO)淋巴瘤诊疗指南-2023[M]. 北京: 人民卫生出版社, 2023. |
| Organized by the Guidelines Working Committee of the Chinese Society of Clinical Oncology. Chinese Society of Clinical Oncology (CSCO) guidelines for diagnosis and treatment of lymphoma-2023[M]. Beijing: People's Health Publishing House, 2023. | |
| [8] | CAMPOS-CARRILLO A, WEITZEL J N, SAHOO P, et al. Circulating tumor DNA as an early cancer detection tool[J]. Pharmacol Ther, 2020, 207: 107458. |
| [9] |
ARGILÉS G, TABERNERO J, LABIANCA R, et al. Localised colon cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2020, 31(10): 1291-1305.
doi: S0923-7534(20)39932-4 pmid: 32702383 |
| [10] |
WALIA A, TUIA J, PRASAD V. Progression-free survival, disease-free survival and other composite end points in oncology: improved reporting is needed[J]. Nat Rev Clin Oncol, 2023, 20(12): 885-895.
doi: 10.1038/s41571-023-00823-5 pmid: 37828154 |
| [11] |
COHEN R, VERNEREY D, BELLERA C, et al. Guidelines for time-to-event end-point definitions in adjuvant randomised trials for patients with localised colon cancer: results of the DATECAN initiative[J]. Eur J Cancer, 2020, 130: 63-71.
doi: S0959-8049(20)30058-7 pmid: 32172199 |
| [12] | LABIANCA R, NORDLINGER B, BERETTA G D, et al. Early colon cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2013, 24(Suppl 6): vi64-vi72. |
| [13] | BENSON A B 3rd, SCHRAG D, SOMERFIELD M R, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage Ⅱ colon cancer[J]. J Clin Oncol, 2004, 22(16): 3408-3419. |
| [14] |
TARAZONA N, GIMENO-VALIENTE F, GAMBARDELLA V, et al. Targeted next-generation sequencing of circulating-tumor DNA for tracking minimal residual disease in localized colon cancer[J]. Ann Oncol, 2019, 30(11): 1804-1812.
doi: S0923-7534(20)32598-9 pmid: 31987087 |
| [15] |
MALLA M, LOREE J M, KASI P M, et al. Using circulating tumor DNA in colorectal cancer: current and evolving practices[J]. J Clin Oncol, 2022, 40(24): 2846-2857.
doi: 10.1200/JCO.21.02615 pmid: 35839443 |
| [16] |
UENO H, KAJIWARA Y, SHIMAZAKI H, et al. New criteria for histologic grading of colorectal cancer[J]. Am J Surg Pathol, 2012, 36(2): 193-201.
doi: 10.1097/PAS.0b013e318235edee pmid: 22251938 |
| [17] |
LIEBIG C, AYALA G, WILKS J, et al. Perineural invasion is an independent predictor of outcome in colorectal cancer[J]. J Clin Oncol, 2009, 27(31): 5131-5137.
doi: 10.1200/JCO.2009.22.4949 pmid: 19738119 |
| [18] | MANISUNDARAM N, DIBRITO S R, HU C Y, et al. Reporting of circumferential resection margin in rectal cancer surgery[J]. JAMA Surg, 2023, 158(11): 1195-1202. |
| [19] | TREPANIER M, ERKAN A, KOUYOUMDJIAN A, et al. Examining the relationship between lymph node harvest and survival in patients undergoing colectomy for colon adenocarcinoma[J]. Surgery, 2019, 166(4): 639-647. |
| [1] | HUANG Haozhe, CHEN Hong, ZHENG Dezhong, CHEN Chao, WANG Ying, XU Lichao, WANG Yaohui, HE Xinhong, YANG Yuanyuan, LI Wentao. A CT-based radiomics nomogram for predicting local tumor progression of colorectal cancer lung metastases treated with radiofrequency ablation [J]. China Oncology, 2024, 34(9): 857-872. |
| [2] | WU Wen, ZHANG Ruoxin, WENG Junyong, MA Yanlei, CAI Guoxiang, LI Xinxiang, YANG Yongzhi. Exploring the prognostic value of positive lymph node ratio in stage Ⅲ colorectal cancer patients and establishing a predictive model [J]. China Oncology, 2024, 34(9): 873-880. |
| [3] | GE Zuyin, SONG Kun, LIN Yunxiao, ZHONG Yeling, HAO Jingduo. The feasibility study of FCGBP and BIGH3 in circulating tumor cells as potential markers for colorectal cancer [J]. China Oncology, 2024, 34(8): 745-752. |
| [4] | ZHANG Ruoxin, YE Zilan, WENG Junyong, LI Xinxiang. Correlation study between advanced age and inferior prognosis in stage Ⅱ colorectal cancer patients [J]. China Oncology, 2024, 34(5): 485-492. |
| [5] | LU Yue, LU Renquan, ZHANG Jie, ZHENG Hui. Application value of combined coagulation function indicators in monitoring hypercoagulable state of patients with colorectal cancer after chemotherapy [J]. China Oncology, 2024, 34(3): 278-285. |
| [6] | ZHU Qinyuan, MA Wenjuan, LUAN Jing, WU Wenyu, CHEN Shujun. Efficacy evaluation and influencing factor analysis of 5-aminolevulinic acid photodynamic therapy for Olsen grade 3 actinic keratosis [J]. China Oncology, 2024, 34(12): 1108-1114. |
| [7] | LI Jun, LU Tingwei, FANG Xuqian. Impact of MSI-H/dMMR on clinicopathological characteristics and prognosis of patients with BRAF V600E-mutated resectable colorectal cancer [J]. China Oncology, 2024, 34(11): 1061-1066. |
| [8] | WU Zhibai, XU Guiqin, ZHANG Li, YANG Zhaojuan, LIU Yun, JIAO Kun, CHEN Zehong, XU Chen, ZUO You, ZHENG Ningqian, YE Zhiqian, LIU Yongzhong. Mechanism study of KCMF1 promoting proliferation and NF-κB signaling transduction in colorectal cancer cells [J]. China Oncology, 2024, 34(11): 987-997. |
| [9] | OUYANG Fei, WANG Yang, CHEN Yu, PEI Guoqing, WANG Ling, ZHANG Yang, SHI Lei. Construction of the prediction model of breast cancer bone metastasis based on machine learning [J]. China Oncology, 2024, 34(10): 903-914. |
| [10] | ZHANG Shaohua, LI Zhening, WANG Wei, WEI Yifan, HONG Yonggang, HAO Liqiang. Research progress in the related treatment of KRAS mutant colorectal cancer [J]. China Oncology, 2024, 34(10): 979-986. |
| [11] | Colorectal Cancer Special Committee of Shanghai Anti-Cancer Association . Shanghai plan for early screening, diagnosis and treatment of colorectal cancer (2023 edition) [J]. China Oncology, 2024, 34(1): 13-66. |
| [12] | WU Han, XU Lei, WANG Miaomiao, ZHANG Ruizhe, XU Xiaoyang, GUO Ningjie, WU Shuhua. Correlation of LC3 and the recruitment of dendritic cell and the formation of TLS in colorectal cancer and its clinical significance [J]. China Oncology, 2023, 33(9): 818-828. |
| [13] | DONG Hao, QIU Yonggang, WANG Xinbin, YANG Junjie, LOU Cuncheng, YIN Lekang, YE Xiaodan. Predictive value of logistic regression model based on high-resolution CT signs for high-grade pattern in stage ⅠA lung adenocarcinoma [J]. China Oncology, 2023, 33(8): 768-775. |
| [14] | ZHOU Cong, HE Lina, CHENG Xiaojiao, HUANG Tinglei, TU Shuiping. Effect of RSPO3 on inhibiting the growth of colorectal cancer transplanted tumors and increasing NK cell infiltration in vivo [J]. China Oncology, 2023, 33(7): 664-672. |
| [15] | YE Junling, ZHENG Xiaoying, GUO Xinjian, CHEN Ruihui, YANG Liu, GOU Xiaodan, JIANG Hanmei. A study on mechanism of lncRNA-mediated SNHG5/miR-26a-5p/MTDH signal axis promoting metastasis of colorectal cancer [J]. China Oncology, 2023, 33(7): 673-685. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
