Welcome to China Oncology,
China Oncology ›› 2025, Vol. 35 ›› Issue (3): 320-325.doi: 10.19401/j.cnki.1007-3639.2025.03.008
• Article • Previous Articles Next Articles
SONG Dan( ), CHAI Yaxin, GE Yanping
), CHAI Yaxin, GE Yanping
Received:2024-11-12
Revised:2025-02-05
Online:2025-03-30
Published:2025-04-10
Contact:
SONG Dan
Supported by:Share article
CLC Number:
SONG Dan, CHAI Yaxin, GE Yanping. Relationship between quantitative analysis parameters of DCE-MRI and microangiogenesis in rectal cancer[J]. China Oncology, 2025, 35(3): 320-325.
Tab. 1
Comparison of DCE-MRI quantitative analysis parameters and MVD in cancer tissues and adjacent tissues ($\bar{x}\pm s$)"
| Tissue | Kep value/min | Ktrans value/min | Ve value | MVD |
|---|---|---|---|---|
| Rectal cancer tissue (n=348) | 2.61±0.59 | 0.84±0.17 | 0.63±0.14 | 30.69±5.27 |
| Adjacent peritumoral tissues (n=348) | 1.57±0.36 | 0.43±0.12 | 0.31±0.11 | 18.72±4.81 |
| t value | 28.070 | 36.756 | 33.528 | 31.296 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |

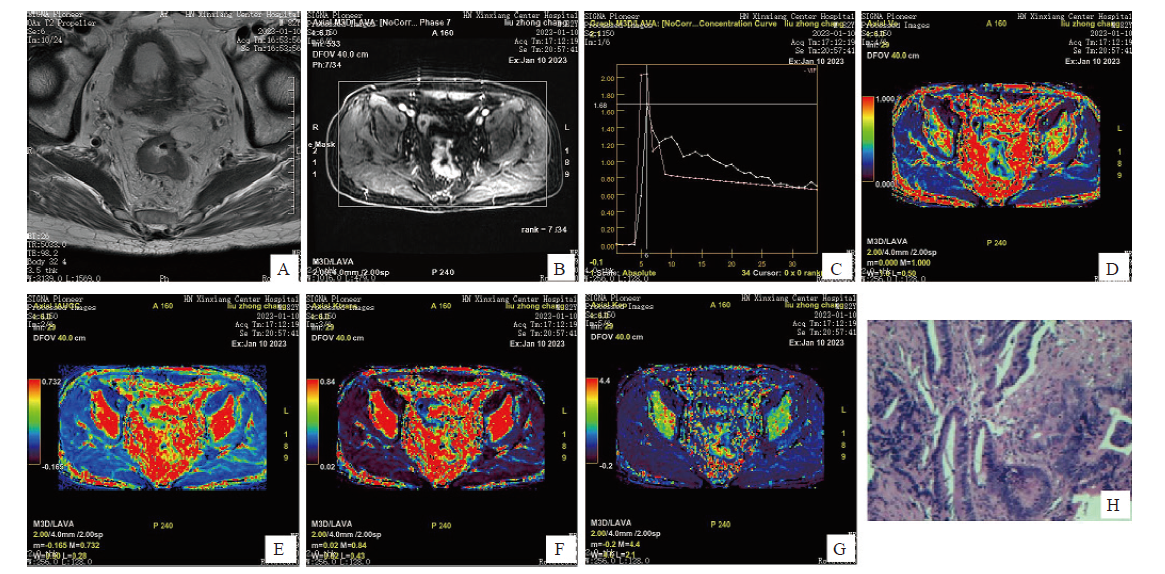
Fig. 1
DCE-MRI image and postoperative pathology image An 82-year-old male presented with anal distension and retraction for six months, and was subsequently diagnosed with rectal cancer by pathological examination. A: The intestinal wall in the middle and lower part of rectum is unevenly thickened, with slightly high signal on T2WI, and the lesion penetrates the muscularis propria; B: The lesion showed uneven and continuous enhancement; C: Time-signal intensity curve of DCE-MRI (pink is the lesion curve); D: Pseudo-color image, yellow-green area shows local occupation of intestinal wall; E, F: Pseudo-color image, red area shows local occupation of intestinal wall; G: Pseudo-color image, with red and yellow areas showing local occupation of intestinal wall; H: Postoperative pathological picture, diagnosed as rectal (H-E staining, ×200)."
Tab. 2
Comparison of DCE-MRI parameters and MVD of rectal cancer patients with different degrees of differentiation ($\bar{x}\pm s$)"
| Degree of differentiation | Kep value/min | Ktrans value/min | Ve value | MVD |
|---|---|---|---|---|
| Highly differentiation (n=68) | 2.04±0.41 | 0.52±0.13 | 0.38±0.12 | 23.46±5.73 |
| Moderate differentiation (n=174) | 2.53±0.53a | 0.83±0.19a | 0.59±0.19a | 30.18±6.09a |
| Poorly differentiation (n=106) | 3.11±0.65ab | 1.06±0.24ab | 0.87±0.26ab | 39.25±6.81ab |
| t value | 82.271 | 155.608 | 128.129 | 141.469 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
Tab. 3
Comparison of DCE-MRI parameters and MVD of rectal cancer patients in different clinical stages ($\bar{x}\pm s$)"
| Clinical stage | Kep value/min | Ktrans value/min | Ve value | MVD |
|---|---|---|---|---|
| Ⅰ (n=79) | 1.91±0.43 | 0.51±0.17 | 0.37±0.11 | 22.87±4.65 |
| Ⅱ (n=116) | 2.42±0.51a | 0.83±0.21a | 0.56±0.15a | 28.65±5.79a |
| Ⅲ (n=88) | 2.87±0.62ab | 0.94±0.26ab | 0.75±0.24ab | 32.40±6.51ab |
| Ⅳ (n=65) | 3.45±0.74abc | 1.12±0.31abc | 0.91±0.28abc | 41.52±7.38abc |
| t value | 96.258 | 86.430 | 103.774 | 118.998 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
Tab. 4
Correlation between DCE-MRI parameters and differentiation degree, clinical stage and MVD in patients with rectal cancer"
| DCE-MRI parameter | Degree of differentiation | Clinical stages | MVD | |||
|---|---|---|---|---|---|---|
| r value | P value | r value | P value | r value | P value | |
| Kep value | -0.683 | 0.008 | 0.764 | <0.001 | 0.812 | <0.001 |
| Ktrans value | -0.743 | <0.001 | 0.703 | <0.001 | 0.754 | <0.001 |
| Ve value | -0.721 | <0.001 | 0.814 | <0.001 | 0.835 | <0.001 |
| [1] |
LYNCH P, RYAN O K, DONNELLY M, et al. Comparing neoadjuvant therapy followed by local excision to total mesorectal excision in the treatment of early stage rectal cancer: a systematic review and meta-analysis of randomised clinical trials[J]. Int J Colorectal Dis, 2023, 38(1): 263.
doi: 10.1007/s00384-023-04558-8 pmid: 37924372 |
| [2] | FAROOQI M, HUSSAIN A, AHMAD A, et al. Impact of trans-anal versus laparoscopic total mesorectal excision on the surgical and pathologic outcomes of patients with rectal cancer: meta-analysis of randomized controlled trials[J]. Langenbecks Arch Surg, 2023, 408(1): 413. |
| [3] | PERIVOLIOTIS K, NTELLAS P, DADOULI K, et al. Microvessel density (MVD) in patients with osteosarcoma: a systematic review and meta-analysis[J]. Cancer Invest, 2024, 42(1): 104-114. |
| [4] | JIANG J J, LI J Z, XIONG X Y, et al. Different predictive values of microvessel density for biochemical recurrence among different PCa populations: a systematic review and meta-analysis[J]. Cancer Med, 2023, 12(3): 2166-2178. |
| [5] | 柴亚欣, 牛永超. 动态对比增强MRI联合体素内不相干运动术前评估直肠癌病理分型[J]. 中国医学影像技术, 2023, 39(12): 1833-1837. |
| CHAI Y X, NIU Y C. Dynamic contrast enhanced MRI combined with intravoxel incoherent motion for preoperative evaluation on pathological type of rectal cancer[J]. Chin J Med Imag Technol, 2023, 39(12): 1833-1837. | |
| [6] | ARIAN A, SEYED-KOLBADI F Z, YAGHOOBPOOR S, et al. Diagnostic accuracy of intravoxel incoherent motion (IVIM) and dynamic contrast-enhanced (DCE) MRI to differentiate benign from malignant breast lesions: a systematic review and meta-analysis[J]. Eur J Radiol, 2023, 167: 111051. |
| [7] | 汪洁, 包善磊, 胡月, 等. 动态对比增强磁共振成像影像组学评估胶质瘤异柠檬酸脱氢酶1突变与微血管生成[J]. 放射学实践, 2023, 38(6): 685-692. |
| WANG J, BAO S L, HU Y, et al. Evaluation of IDH1 mutation and angiogenesis in gliomas by radiomics analysis based on DCE-MRI[J]. Radiol Pract, 2023, 38(6): 685-692. | |
| [8] | SHINAGAWA T, TANAKA T, NOZAWA H, et al. Comparison of the guidelines for colorectal cancer in Japan, the USA and Europe[J]. Ann Gastroenterol Surg, 2017, 2(1): 6-12. |
| [9] | 李玉林. 病理学[M]. 7版. 北京: 人民卫生出版社, 2008: 79-80. |
| LI Y L. Pathology[M]. 7 Edition. Beijing: People’s Medical Publishing House, 2008: 79-80. | |
| [10] | TONG G J, ZHANG G Y, LIU J, et al. Comparison of the eighth version of the American Joint Committee on Cancer manual to the seventh version for colorectal cancer: a retrospective review of our data[J]. World J Clin Oncol, 2018, 9(7): 148-161. |
| [11] |
WEIDNER N, FOLKMAN J, POZZA F, et al. Tumor angiogenesis: a new significant and independent prognostic indicator in early-stage breast carcinoma[J]. J Natl Cancer Inst, 1992, 84(24): 1875-1887.
doi: 10.1093/jnci/84.24.1875 pmid: 1281237 |
| [12] | PELTRINI R, IMPERATORE N, DI NUZZO M M, et al. Towards personalized treatment of T2N0 rectal cancer: a systematic review of long-term oncological outcomes of neoadjuvant therapy followed by local excision[J]. J Gastroenterol Hepatol, 2022, 37(8): 1426-1433. |
| [13] |
TAN S F, GAO Q Q, CUI Y P, et al. Oncologic outcomes of watch-and-wait strategy or surgery for low to intermediate rectal cancer in clinical complete remission after adjuvant chemotherapy: a systematic review and meta-analysis[J]. Int J Colorectal Dis, 2023, 38(1): 246.
doi: 10.1007/s00384-023-04534-2 pmid: 37787779 |
| [14] | PERIVOLIOTIS K, SAMARA A A, KOUTOUKOGLOU P, et al. Microvessel density in differentiated thyroid carcinoma: a systematic review and meta-analysis[J]. World J Methodol, 2022, 12(5): 448-458. |
| [15] | 牛涛, 燕翠芳. DCE-MRI联合弥散加权成像对老年直肠癌诊断价值及术前分期评估[J]. 中国老年学杂志, 2024, 44(19): 4645-4647. |
| NIU T, YAN C F. Diagnostic value and preoperative staging evaluation of DCE-MRI combined with diffusion-weighted imaging in elderly rectal cancer[J]. Chin J Gerontol, 2024, 44(19): 4645-4647. | |
| [16] | ARIAN A, TAHER H J, SUHAIL NAJM ALAREER H, et al. Value of conventional MRI, DCE-MRI, and DWI-MRI in the discrimination of metastatic from non-metastatic lymph nodes in rectal cancer: a systematic review and meta-analysis study[J]. Asian Pac J Cancer Prev, 2023, 24(2): 401-410. |
| [17] | 吕霞, 刘强, 刘岘, 等. 直肠癌DCE-MRI定量参数与病理分化程度和p53的相关性[J]. 实用医学杂志, 2022, 38(4): 479-483. |
| LÜ X, LIU Q, LIU X, et al. An analysis on association of DCE-MRI quantitative parameters with pathological differentiation and p53 in rectal cancer[J]. J Pract Med, 2022, 38(4): 479-483. | |
| [18] |
MULYADI R, PUTRI P P, HANDOKO H, et al. Dynamic contrast-enhanced magnetic resonance imaging parameter changes as an early biomarker of tumor responses following radiation therapy in patients with spinal metastases: a systematic review[J]. Radiat Oncol J, 2023, 41(4): 225-236.
doi: 10.3857/roj.2023.00290 pmid: 38185927 |
| [19] | 杨彦松, 李君, 张明珠, 等. DCE-MRI定量参数联合高分辨率T2WI预测直肠腺癌病理N分期的价值[J]. 放射学实践, 2023, 38(4): 459-467. |
| YANG Y S, LI J, ZHANG M Z, et al. Value of quantitative parameters of dynamic contrast-enhanced MRI combined with high-resolution T2WI findings in predicting pathological N-stage of rectal adenocarcinoma[J]. Radiol Pract, 2023, 38(4): 459-467. | |
| [20] |
ZHANG J, WANG L, LIU H F. Imaging features derived from dynamic contrast-enhanced magnetic resonance imaging to differentiate malignant from benign breast lesions: a systematic review and meta-analysis[J]. J Comput Assist Tomogr, 2022, 46(3): 383-391.
doi: 10.1097/RCT.0000000000001289 pmid: 35575651 |
| [21] | SHOMAL ZADEH F, POOYAN A, ALIPOUR E, et al. Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) in differentiation of soft tissue sarcoma from benign lesions: a systematic review of literature[J]. Skeletal Radiol, 2024, 53(7): 1343-1357. |
| [22] | 杨炼, 肖明, 李娴, 等. 人结直肠癌组织及LOVO细胞中ARTC1的表达及其与肿瘤微血管生成的相关性[J]. 临床与实验病理学杂志, 2022, 38(10): 1198-1203. |
| YANG L, XIAO M, LI X, et al. Expression of ARTC1 in human colorectal cancer tissues and LOVO cells and its relationship with microangiogenesis[J]. Chin J Clin Exp Pathol, 2022, 38(10): 1198-1203. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
沪ICP备12009617
Powered by Beijing Magtech Co. Ltd
